From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate, Then Clot Blood Cells in Pulmonary and Systemic Microvasculature
PhD David E Scheim
The role of vascular occlusion in the morbidities, pulmonary and systemic, of COVID-19 has received increasing focus. Histological studies of lung tissue from COVID-19 patients have found extensively damaged endothelium of capillaries adjoining relatively intact alveoli, corresponding to hypoxemia accompanying normal breathing mechanics in such patients. Essential to the study of vascular occlusion in COVID-19 are viral properties dating back to studies of Jonas Salk in the 1940s that have been positively established for SARS-CoV-2. First, SARS-CoV-2 binds to red blood cells (RBCs) in vitro and also clinically in COVID-19 patients. Second, although fusion and replication of SARS-CoV-2 occur via ACE2, such hemagglutinating viruses initially attach to infective targets and clump with blood cells via much more abundantly distributed glycoconjugate binding sites, notably those tipped with sialic acid (SA). SARS-CoV-2, in particular, attaches to these glycan binding sites. Third, certain enveloped viruses express an enzyme, hemagglutinin esterase (HE), that counteracts viral-RBC clumping. Notably, among betacoronaviruses, the common cold strains express HE while SARS-CoV-2, SARS-CoV-1 and MERS, the virulent strains, do not. The hemagglutinating properties of SARS-COV-2 establish a framework for "catch and clump" induction of microvascular occlusion proposed here. Ultramicroscopic studies of tissues from COVID-19 patients indicate a key role for hemagglutination early and mid-course in COVID-19, before such clumps develop into clots via the coagulation cascade.
References
Ackermann, Verleden, Kuehnel, Haverich, Welte et al., Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19, N Engl J Med
Ackerstaff, Keunen, Wv, Admv, Stijnen, Influence of biological factors on changes in mean cerebral blood flow velocity in normal ageing: a transcranial Doppler study, Neurological Research
Adams, Kuhnrae, Higgins, Ghumra, Rowe, Rosetting Plasmodium falciparum-infected erythrocytes bind to human brain microvascular endothelial cells in vitro, demonstrating a dual adhesion phenotype mediated by distinct P. falciparum erythrocyte membrane protein 1 domains, Infect Immun
Adams, Sim, Dolan, Fang, Kaslow et al., A family of erythrocyte binding proteins of malaria parasites, Proc Natl Acad Sci
Agafonov, Aa, Ternovoi, Ryabchikova, Durymanov et al., Primary characterization of SARS coronavirus strain Frankfurt 1, Dokl Biol Sci
Aguiar, Tremblay, Mansfield, Woody, Lobb et al., Gene expression and in situ protein profiling of candidate SARS-CoV-2 receptors in human airway epithelial cells and lung tissue, European Respiratory Journal
Ahmetaj-Shala, Vaja, Atanur, George, Kirkby et al., Systemic analysis of putative SARS-CoV-2 entry and processing genes in cardiovascular tissues identifies a positive correlation of BSG with age in endothelial cells, bioRxiv,
doi:10.1101/2020.06.23.165324.128Allain, Vanpouille, Carpentier, Slomianny, Durieux et al., Interaction with glycosaminoglycans is required for cyclophilin B to trigger integrin-mediated adhesion of peripheral blood T lymphocytes to extracellular matrix, Proceedings of the National Academy of Sciences
Anderson, Brodsky, Mangalmurti, The Evolving Erythrocyte: Red Blood Cells as Modulators of Innate Immunity, J Immunol
Antoniak, Mackman, Multiple roles of the coagulation protease cascade during virus infection, Blood
Antoniak, The coagulation system in host defense, Res Pract Thromb Haemost
Aoki, A Comprehensive Review of Our Current Understanding of Red Blood Cell (RBC) Glycoproteins, Membranes
Arman, Rowe, Experimental conditions affect the outcome of Plasmodium falciparum plateletmediated clumping assays, Malar J
Arora, Gwinn, Bower, Watson, Okwumabua et al., Extracellular cyclophilins contribute to the regulation of inflammatory responses, J Immunol
Assinger, Platelets and Infection -An Emerging Role of Platelets in Viral Infection, Frontiers in Immunology
Awasthi, Gulati, Sarkar, Tiwari, Kateriya et al., The Sialoside-Binding Pocket of SARS-CoV-2 Spike Glycoprotein Structurally Resembles MERS-CoV, Viruses
Back, Kostova, Klei, Beuger, Van Zwieten et al., RBC Adhesive Capacity Is Essential for Efficient 'Immune Adherence Clearance' and Provide a Generic Target to Deplete Pathogens from Septic Patients, Blood
Backer, Lins, Dierckx, Vandevenne, Backer et al., CT-derived measurements of pulmonary blood volume in small vessels and need for oxygen in COVID-19 patients, medRxiv,
doi:10.1101/2020.06.03.20121483.226Bai, Huang, Ma, Jiang, Chen, Importance of N-glycosylation on CD147 for its biological functions, Int J Mol Sci
Baker, Richards, Guy, Congdon, Hasan et al., The SARS-COV-2 Spike Protein Binds Sialic Acids and Enables Rapid Detection in a Lateral Flow Point of Care Diagnostic Device, ACS Central Science
Bakkers, Lang, Feitsma, Hulswit, De Poot et al., Betacoronavirus Adaptation to Humans Involved Progressive Loss of Hemagglutinin-Esterase Lectin Activity, Cell Host & Microbe
Bakkers, Zeng, Feitsma, Hulswit, Li et al., Coronavirus receptor switch explained from the stereochemistry of protein-carbohydrate interactions and a single mutation, Proc Natl Acad Sci
Bao, Twigg, Shackel, Warner, Yue, Monocyte CD147 is induced by advanced glycation end products and high glucose concentration: possible role in diabetic complications, Am J Physiol Cell Physiol
Barrett, Inglis, Growth, purificatin and titratin of influenza viruses
Baskurt, Neu, Meiselman, Red Blood Cell Aggregation
Baum, Ward, Conway, Natural selection on the erythrocyte surface, Mol Biol Evol
Becker, COVID-19 update: Covid-19-associated coagulopathy, J Thromb Thrombolysis
Becker, Sexton, Smyth, Translational Implications of Platelets as Vascular First Responders, Circ Res
Belouzard, Millet, Licitra, Whittaker, Mechanisms of Coronavirus Cell Entry Mediated by the Viral Spike Protein, Viruses
Bernard, Simpson, Join-Lambert, Federici, Laran-Chich et al., Pathogenic Neisseria meningitidis utilizes CD147 for vascular colonization, Nat Med
Berzuini, Bianco, Migliorini, Maggioni, Valenti et al., Red blood cell morphology in patients with COVID-19-related anaemia, Blood Transfus
Bharara, Singh, Pattnaik, Chitnis, Sharma, Structural analogs of sialic acid interfere with the binding of erythrocyte binding antigen-175 to glycophorin A, an interaction crucial for erythrocyte invasion by Plasmodium falciparum, Molecular and Biochemical Parasitology
Bian, Zheng, Wei, Wen, Zhang et al., Safety and efficacy of meplazumab in healthy volunteers and COVID-19 patients: a randomized phase 1 and an exploratory phase 2 trial, Signal Transduction and Targeted Therapy
Bikdeli, Madhavan, Jimenez, Chuich, Dreyfus et al., COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC Stateof-the-Art Review, J Am Coll Cardiol
Blom, Monitoring of Respiration and Circulation
Bossart, Meyer, Bienz, Electron microscopic study on influenza virus hemagglutination: Pinocytosis of virions by red cells, Virology
Bourgonje, Abdulle, Timens, Hillebrands, Navis et al., Angiotensin-converting enzyme-2 (ACE2), SARS-CoV-2 and pathophysiology of coronavirus disease 2019 (COVID-19), J Pathol,
doi:10.1002/path.5471Brian, Hogue, Kienzle, The Coronavirus Hemagglutinin Esterase Glycoprotein
Bubshait, Albuali, Yousef, Obeid, Alkharsah et al., Clinical description of human bocavirus viremia in children with LRTI, Eastern Province, Saudi Arabia, Ann Thorac Med
Bucknall, King, Kapikian, Chanock, Studies with human coronaviruses. II. Some properties of strains 229E and OC43, Proc Soc Exp Biol Med
Carbajo-Lozoya, Ma-Lauer, Malešević, Theuerkorn, Kahlert et al., Human coronavirus NL63 replication is cyclophilin A-dependent and inhibited by non-immunosuppressive cyclosporine A-derivatives including Alisporivir, Virus Res
Carnevale, Beretta, Morbini, Direct endothelial damage and vasculitis due to SARS-CoV-2 in small bowel submucosa of COVID-19 patient with diarrhea, J Med Virol,
doi:10.1002/jmv.26119.204Carsana, Sonzogni, Nasr, Rossi, Pellegrinelli et al., Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy, medRxiv,
doi:10.1101/2020.04.19.20054262.175Chabert, Hamzeh-Cognasse, Pozzetto, Cognasse, Schattner et al., Human platelets and their capacity of binding viruses: meaning and challenges?, BMC Immunology
Chan, Kok, Zhu, Chu, To et al., Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan, Emerging Microbes & Infections
Chen, Gao, Wang, Nguyen, Wei, Review of COVID-19 Antibody Therapies, Annu Rev Biophys
Chen, Hui, Ren, Luo, Shu et al., The N-glycosylation sites and Glycan-binding ability of Sprotein in SARS-CoV-2 Coronavirus, bioRxiv,
doi:10.1101/2020.12.01.406025.113Chen, Lan, Yuan, Deng, Li et al., Detectable 2019-nCoV viral RNA in blood is a strong indicator for the further clinical severity, Emerg Microbes Infect
Chen, Liu, Guo, Emerging coronaviruses: Genome structure, replication, and pathogenesis, J Med Virol
Chen, Mi, Xu, Yu, Wang et al., Function of HAb18G/CD147 in invasion of host cells by severe acute respiratory syndrome coronavirus, J Infect Dis
Cohen, Varki, Chapter Three -Modulation of Glycan Recognition by Clustered Saccharide Patches, International Review of Cell and Molecular Biology
Collins, Blixt, Desieno, Bovin, Marth et al., Masking of CD22 by cis ligands does not prevent redistribution of CD22 to sites of cell contact, Proc Natl Acad Sci
Collins, Paulson, Cell surface biology mediated by low affinity multivalent protein-glycan interactions, Current Opinion in Chemical Biology
Colmenero, Santonja, Alonso-Riaño, Noguera-Morel, Hernández-Martín et al., SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases, Br J Dermatol
Colpitts, Schang, A Small Molecule Inhibits Virion Attachment to Heparan Sulfate-or Sialic Acid-Containing Glycans, J Virol
Coste, Gauchat, -Fo, Izui, Jeannin et al., Unavailability of CD147 leads to selective erythrocyte trapping in the spleen, Blood
Couzin-Frankel, The mystery of the pandemic's 'happy hypoxia, Science
Crosnier, Bustamante, Bartholdson, Bei, Theron et al., Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum, Nature
Crump, Ōmura, Ivermectin, 'wonder drug' from Japan: the human use perspective, Proc Jpn Acad Ser B Phys Biol Sci
Cserti-Gazdewich, Dhabangi, Musoke, Ssewanyana, Ddungu et al., Cytoadherence in paediatric malaria: ABO blood group, CD36, and ICAM1 expression and severe Plasmodium falciparum infection, British Journal of Haematology
Dai, Zhang, Ostrikov, Abrahamyan, Host receptors: the key to establishing cells with broad viral tropism for vaccine production, Critical Reviews in Microbiology
Daniel, DOD-backed Research Indicates COVID-19 Lasting Symptoms Not Neurological but Result from Small Blood Cells
De Groot, Baker, Baric, Enjuanes, Family -Coronaviridae
De Groot, Structure, function and evolution of the hemagglutinin-esterase proteins of corona-and toroviruses, Glycoconjugate Journal
Defang, Martin, Burgess, Millar, Pecenka et al., Comparative analysis of hemagglutination inhibition titers generated using temporally matched serum and plasma samples, PLoS One
Deroost, Pham, Opdenakker, Van Den Steen, The immunological balance between host and parasite in malaria, FEMS Microbiol Rev
Desforges, Desjardins, Zhang, Talbot, The acetyl-esterase activity of the hemagglutinin-esterase protein of human coronavirus OC43 strongly enhances the production of infectious virus, J Virol
Diez-Silva, Dao, Han, Lim, Suresh, Shape and Biomechanical Characteristics of Human Red Blood Cells in Health and Disease, MRS Bull
Dinenno, Jones, Seals, Tanaka, Limb Blood Flow and Vascular Conductance Are Reduced With Age in Healthy Humans, Circulation
Doumbo, Thera, Koné, Raza, Tempest et al., High levels of Plasmodium falciparum rosetting in all clinical forms of severe malaria in African children, Am J Trop Med Hyg
Duan, Zheng, Zhang, Niu, Lou et al., The SARS-CoV-2 Spike Glycoprotein Biosynthesis, Structure, Function, and Antigenicity: Implications for the Design of Spike-Based Vaccine Immunogens, Frontiers in Immunology
Ellinghaus, Degenhardt, Bujanda, Buti, Albillos et al., Genomewide Association Study of Severe Covid-19 with Respiratory Failure, N Engl J Med
Fajnzylber, Regan, Coxen, Corry, Wong et al., SARS-CoV-2 viral load is associated with increased disease severity and mortality, Nature Communications
Fang, Zhang, Hang, Li, Zhang, Comparisons of viral shedding time of SARS-CoV-2 of different samples in ICU and non-ICU patients, J Infect
Fantini, Scala, Chahinian, Yahi, Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection, International Journal of Antimicrobial Agents
Gagneten, Gout, Dubois-Dalcq, Rottier, Rossen et al., Interaction of mouse hepatitis virus (MHV) spike glycoprotein with receptor glycoprotein MHVR is required for infection with an MHV strain that expresses the hemagglutinin-esterase glycoprotein, J Virol
Gattinoni, Coppola, Cressoni, Busana, Rossi et al., COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome, Am J Respir Crit Care Med
Gerdes, Klein, Devald, Burks, Coronavirus isolates SK and SD from multiple sclerosis patients are serologically related to murine coronaviruses A59 and JHM and human coronavirus OC43, but not to human coronavirus 229E, J Virol
Goeijenbier, Van Wissen, Van De Weg, Gerdes, Meijers, Review: Viral infections and mechanisms of thrombosis and bleeding, J Med Virol
Guest, Bond, Cooper, Derrick, Red Blood Cells: Change in Shape in Capillaries, Science
Guo, Ye, Zhang, Yu, Cui et al., A critical epitope in CD147 facilitates memory CD4(+) T-cell hyper-activation in rheumatoid arthritis, Cell Mol Immunol
Gupta, Madhavan, Sehgal, Nair, Mahajan et al., Extrapulmonary manifestations of COVID-19, Nat Med
Hagman, Hedenstierna, Gille-Johnson, Hammas, Grabbe et al., Viral RNA load in plasma is associated with critical illness and a dysregulated host response in COVID-19, Clin Infect Dis,
doi:10.1093/cid/ciaa1285Halbhuber, Gliesing, Stibenz, Makovitzky, Topo-optical investigations of the human erythrocyte glycocalyx-age related changes, Histochemistry
Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study, Intensive Care Med
Hemphill, Frame, Ross, The interaction of Trypanosoma congolense with endothelial cells, Parasitology
Hierholzer, Purification and biophysical properties of human coronavirus 229, E. Virology
Hierholzer, Suggs, Hall, Standardized viral hemagglutination and hemagglutination-inhibition tests. II. Description and statistical evaluation, Appl Microbiol
Hirst, Adsorption of influenza hemagglutinins and virus by red blood cells, Journal of Experimental Medicine
Hirst, The agglutination of red cells by allantoic fluid of chick embryos infected with influenza virus, Science
Howe, Lee, Virus-Erythrocyte Interactions
Huang, Chen, Yang, Guan, Liu et al., SARS-CoV-2 Viral Load in Clinical Samples from Critically Ill Patients, American Journal of Respiratory and Critical Care Medicine
Huang, Dong, Milewska, Qi, Zhu, Human Coronavirus HKU1 Spike Protein Uses O-Acetylated Sialic Acid as an Attachment Receptor Determinant and Employs Hemagglutinin-Esterase Protein as a Receptor-Destroying Enzyme, J Virol
Huertas, Montani, Savale, Pichon, Tu et al., Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)?, Eur Respir J
Hulswit, De Haan, Bosch, Chapter Two -Coronavirus Spike Protein and Tropism Changes, Advances in Virus Research
Hulswit, Lang, Bakkers, Li, Li et al., Human coronaviruses OC43 and HKU1 bind to 9-O-acetylated sialic acids via a conserved receptor-binding site in spike protein domain A, Proc Natl Acad Sci
Hurlburt, Seydoux, Wan, Edara, Stuart et al., Structural basis for potent neutralization of SARS-CoV-2 and role of antibody affinity maturation, Nature Communications
Hussien, Abdelaziz, Molecular docking suggests repurposing of brincidofovir as a potential drug targeting SARS-CoV-2 ACE2 receptor and main protease, Network Modeling Analysis in Health Informatics and Bioinformatics
Hyvärinen, Meri, Jokiranta, Disturbed sialic acid recognition on endothelial cells and platelets in complement attack causes atypical hemolytic uremic syndrome, Blood
Islam, Islam, Haque, Rahman, Thermal and pH sensitivity of avian corona and influenza viruses: A model study for inactivation of SARS-CoV-2 (COVID-19) and other flu viruses, International Research Journal of Medicine and Medical Sciences
Ivanova, Devlin, Buus, Koide, Shwetar et al., SARS-CoV-2 mRNA vaccine elicits a potent adaptive immune response in the absence of IFN-mediated inflammation observed in COVID-19, medRxiv,
doi:10.1101/2021.04.20.21255677.256Jaskiewicz, Jodłowska, Kaczmarek, Zerka, Erythrocyte glycophorins as receptors for Plasmodium merozoites, Parasites & Vectors
Johansson, The Role of the Endothelial Cell Surface Charge for Blood-Brain Barrier Function
Jose, Manuel, COVID-19 cytokine storm: the interplay between inflammation and coagulation, Lancet Respir Med
Joseph, Knobler, Lublin, Burns, Telen, Regulation of the expression of intercellular adhesion molecule-1 (ICAM-1) and the putative adhesion molecule Basigin on murine cerebral endothelial cells by MHV-4 (JHM), Seminars in Hematology
Jung, Krüger-Genge, Franke, Hufert, Küpper, COVID-19 and the endothelium, Clinical Hemorheology and Microcirculation
Jötten, Moll, Wahlgren, Wixforth, Westerhausen, Blood group and size dependent stability of P. falciparum infected red blood cell aggregates in capillaries, Biomicrofluidics
Kalhor, Sadeghi, Abolhasani, Kalhor, Rahimi, Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics,
doi:10.1080/07391102.2020.1824816:1-16.264Kapikian, James, Kelly, King, Vaughn et al., Hemadsorption by coronavirus strain OC43, Proc Soc Exp Biol Med
Kasinrerk, Tokrasinwit, Phunpae, CD147 monoclonal antibodies induce homotypic cell aggregation of monocytic cell line U937 via LFA-1/ICAM-1 pathway, Immunology
Kaur, Shekhar, Sharma, Sarma, Prakash et al., Ivermectin as a potential drug for treatment of COVID-19: an in-sync review with clinical and computational attributes, Pharmacological Reports,
doi:10.1007/s43440-020-00195-y.271Kendal, A comparison of "influenza C" with prototype myxoviruses: Receptor-destroying activity (neuraminidase) and structural polypeptides, Virology
Killian, Hemagglutination Assay for Influenza Virus
Koch, Staffler, Hüttinger, Hilgert, Prager et al., T cell activation-associated epitopes of CD147 in regulation of the T cell response, and their definition by antibody affinity and antigen density, Int Immunol
Koehler, Delguste, Sieben, Gillet, Alsteens, Initial Step of Virus Entry: Virion Binding to Cell-Surface Glycans, Annual Review of Virology
Krejza, Mariak, Walecki, Szydlik, Lewko et al., Transcranial color Doppler sonography of basal cerebral arteries in 182 healthy subjects: age and sex variability and normal reference values for blood flow parameters, AJR Am J Roentgenol
Kuchel, Shishmarev, Accelerating metabolism and transmembrane cation flux by distorting red blood cells, Science Advances
Kumar, Nyodu, Maurya, Saxena, Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
Kwon, Oh, Kwon, Zhang, Fraser, Sulfated polysaccharides effectively inhibit SARS-CoV-2 in vitro, Cell Discovery
Lakhdari, Tabet, Boudraham, Laoussati, Aissanou et al., Red blood cells injuries and hypersegmented neutrophils in COVID-19 peripheral blood film, medRxiv,
doi:10.1101/2020.07.24.20160101.278Lam, Murphy, Kuri-Cervantes, Weisman, Ittner et al., Erythrocytes Reveal Complement Activation in Patients with COVID-19, medRxiv,
doi:10.1101/2020.05.20.20104398Lang, Li, Li, Koerhuis, Van Den Burg et al., Coronavirus hemagglutinin-esterase and spike proteins coevolve for functional balance and optimal virion avidity, Proc Natl Acad Sci
Langereis, Van Vliet, Boot, De Groot, Attachment of mouse hepatitis virus to O-acetylated sialic acid is mediated by hemagglutinin-esterase and not by the spike protein, J Virol
Lehrer, Rheinstein, Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, Vivo
Levine, Levine, Sharp, Brooks, Theory of the electrokinetic behavior of human erythrocytes, Biophysical Journal
Li, Hulswit, Widjaja, Raj, Mcbride et al., Identification of sialic acid-binding function for the Middle East respiratory syndrome coronavirus spike glycoprotein, Proc Natl Acad Sci
Li, Liu, Ge, Scientific research progress of COVID-19/SARS-CoV-2 in the first five months, Journal of Cellular and Molecular Medicine
Liao, Klaus, Neumann, Control of Innate Immunity by Sialic Acids in the Nervous Tissue, Int J Mol Sci
Libby, Lüscher, COVID-19 is, in the end, an endothelial disease, European Heart Journal
Lins, Vandevenne, Thillai, Lavon, Lanclus et al., Assessment of Small Pulmonary Blood Vessels in COVID-19 Patients Using HRCT, Acad Radiol
Liu, Chopra, Li, Wolfert, Tompkins et al., SARS-CoV-2 spike protein binds heparan sulfate in a length-and sequence-dependent manner, bioRxiv,
doi:10.1101/2020.05.10.087288Lodigiani, Lapichino, Carenzo, Cecconi, Ferrazzi et al., Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy, Thromb Res
Loh, The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding, Melatonin Research
Lv, Miao, Zhao, Luo, Han et al., CD147-mediated chemotaxis of CD4(+)CD161(+) T cells may contribute to local inflammation in rheumatoid arthritis, Clin Rheumatol
Maeda, Seike, Kon, Shiga, Erythrocyte Aggregation as a Determinant of Blood Flow: Effect of pH, Temperature and Osmotic Pressure,
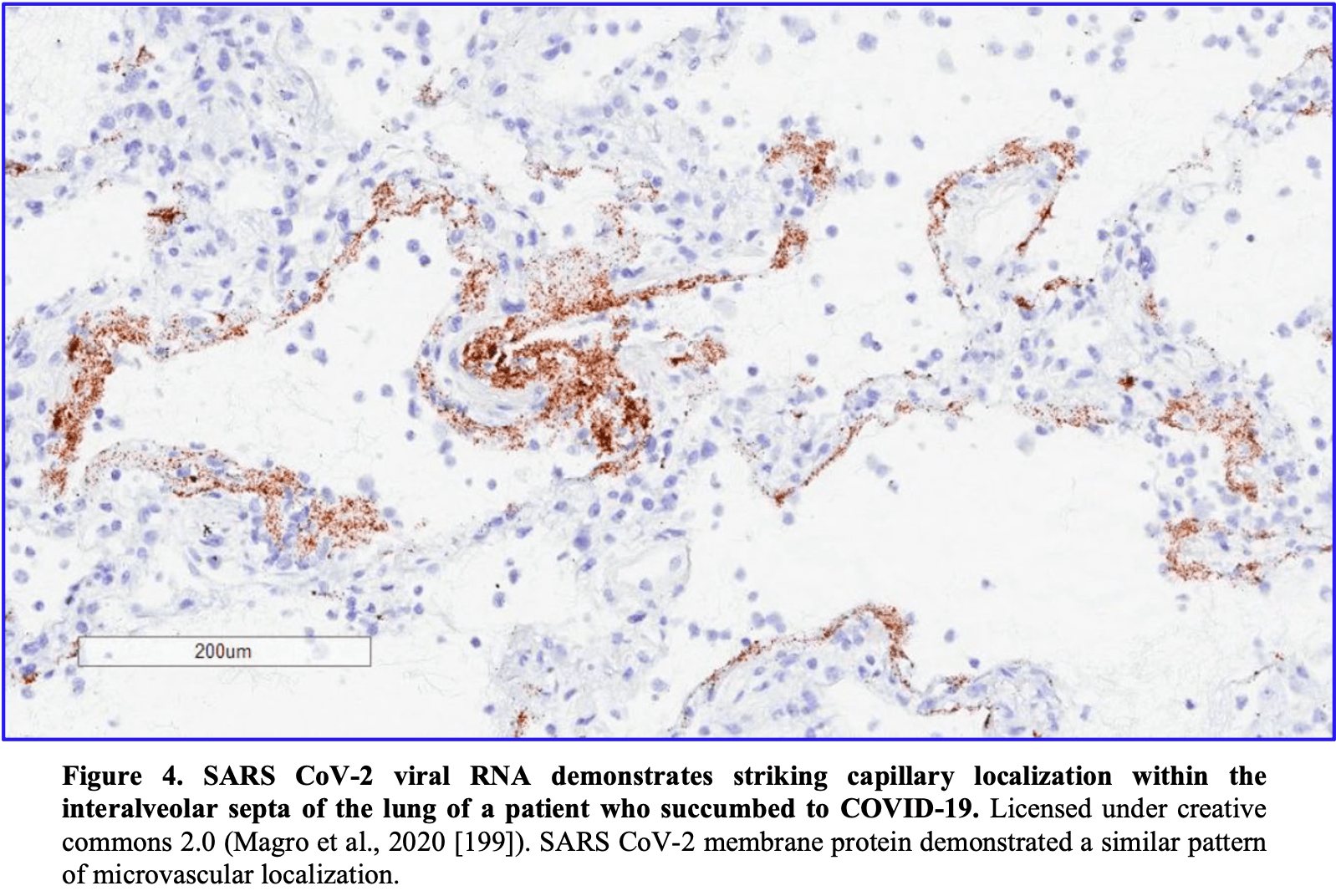
doi:10.1007/978-1-4615-9510-6_68Magro, Mulvey, Berlin, Nuovo, Salvatore et al., Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases, Transl Res
Magro, Mulvey, Laurence, Sanders, Crowson et al., The differing pathophysiologies that underlie COVID-19 associated perniosis and thrombotic retiform purpura: a case series, Br J Dermatol,
doi:10.1111/bjd.19415.200Marini, Gattinoni, Management of COVID-19 Respiratory Distress, JAMA
Matrosovich, Herrler, Klenk, Sialic Acid Receptors of Viruses
Maurya, A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, ChemRxiv,
doi:10.26434/chemrxiv.12630539.v1.272Mcclelland, Hare, The Adsorption of Influenza Virus by Red Cells and a New in vitro Method of Measuring Antibodies for Influenza Virus, Canadian Public Health Journal
Mcquaid, Rowe, Rosetting revisited: a critical look at the evidence for host erythrocyte receptors in Plasmodium falciparum rosetting, Parasitology
Melkumyants, Buryachkovskaya, Lomakin, Antonova, Serebruany, Mild COVID-19 and Impaired Blood Cell-Endothelial Crosstalk: Considering Long-Term Use of Antithrombotics?, Thromb Haemost
Menter, Haslbauer, Nienhold, Savic, Hopfer et al., Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction, Histopathology
Mercurio, Tragni, Busto, Grassi, Pierri, Protein structure analysis of the interactions between SARS-CoV-2 spike protein and the human ACE2 receptor: from conformational changes to novel neutralizing antibodies, Cellular and molecular life sciences : CMLS
Middeldorp, Coppens, Van Haaps, Foppen, Vlaar et al., Incidence of venous thromboembolism in hospitalized patients with COVID-19, J Thromb Haemost
Mikami, Miyashita, Yamada, Harrington, Steinberg et al., Risk Factors for Mortality in Patients with COVID-19 in New York City, Journal of General Internal Medicine,
doi:10.1007/s11606-020-05983-z.228Milanetti, Miotto, Rienzo, Monti, Gosti et al., In-Silico evidence for two receptors based strategy of SARS-CoV-2, bioRxiv,
doi:10.1101/2020.03.24.006197Milewska, Zarebski, Nowak, Stozek, Potempa et al., Human coronavirus NL63 utilizes heparan sulfate proteoglycans for attachment to target cells, J Virol
Mitnaul, Matrosovich, Castrucci, Tuzikov, Bovin et al., Balanced Hemagglutinin and Neuraminidase Activities Are Critical for Efficient Replication of Influenza A Virus, J Virol
Miyagi, Yamaguchi, 3.17 -Sialic Acids
Modrof, Kerschbaum, Farcet, Niemeyer, Corman et al., SARS-CoV-2 and the safety margins of cell-based biological medicinal products, Biologicals
Mondal, Lahiri, Deb, Bandyopadhyay, Shome et al., COVID-19: Are we dealing with a multisystem vasculopathy in disguise of a viral infection?, J Thromb Thrombolysis
Morniroli, Giannì, Consales, Pietrasanta, Mosca, Human Sialome and Coronavirus Disease-2019 (COVID-19) Pandemic: An Understated Correlation?, Frontiers in Immunology
Muramatsu, Basigin (CD147), a multifunctional transmembrane glycoprotein with various binding partners, J Biochem
Nallusamy, Mannu, Ravikumar, Angamuthu, Nathan et al., Shortlisting Phytochemicals Exhibiting Inhibitory Activity against Major Proteins of SARS-CoV-2 through Virtual Screening, Research Square,
doi:10.21203/rs.3.rs-31834/v1.262Negri, Piloto, Morinaga, Jardim, Lamy et al., Heparin Therapy Improving Hypoxia in COVID-19 Patients -A Case Series, Frontiers in Physiology
Nelson, Immune Adherence, Advances in Immunology
Nelson, The Immune-Adherence Phenomenon: An Immunologically Specific Reaction Between Microorganisms and Erythrocytes Leading to Enhanced Phagocytosis, Science
Nelson, The immune-adherence phenomenon; a hypothetical role of erythrocytes in defence against bacteria and viruses, Proc R Soc Med
Neu, Bauer, Stehle, Viruses and sialic acids: rules of engagement, Curr Opin Struct Biol
Newton, Delguste, Koehler, Dumitru, Laskowski et al., Combining confocal and atomic force microscopy to quantify single-virus binding to mammalian cell surfaces, Nature Protocols
Nguyen, Fries, Khoury, Zheng, Hu et al., Automated Imaging and Analysis of the Hemagglutination Inhibition Assay, Journal of Laboratory Automation
Nissilä, Hakala, Leskinen, Roig, Syed et al., Complement Factor H and Apolipoprotein E Participate in Regulation of Inflammation in THP-1 Macrophages, Frontiers in Immunology
Ocak, Kara, Ince, Monitoring microcirculation, Best Practice & Research Clinical Anaesthesiology
Odièvre, Bony, Benkerrou, Lapouméroulie, Alberti et al., Modulation of erythroid adhesion receptor expression by hydroxyurea in children with sickle cell disease, Haematologica
Ogata, Maley, Wu, Gilboa, Norman et al., Ultra-sensitive Serial Profiling of SARS-CoV-2 Antigens and Antibodies in Plasma to Understand Disease Progression in COVID-19 Patients with Severe Disease, Clin Chem,
doi:10.1093/clinchem/hvaa213.217Ombrello, Block, Morrell, Our expanding view of platelet functions and its clinical implications, J Cardiovasc Transl Res
Park, Walls, Wang, Sauer, Li et al., Structures of MERS-CoV spike glycoprotein in complex with sialoside attachment receptors, Nature Structural & Molecular Biology
Pawlotsky, SARS-CoV-2 pandemic : Time to revive the cyclophilin inhibitor alisporivir, Clinical Infectious Diseases,
doi:10.1093/cid/ciaa587.195Pedersen, Hemagglutination-Inhibition Assay for Influenza Virus Subtype Identification and the Detection and Quantitation of Serum Antibodies to Influenza Virus
Peng, Liu, Xu, Luo, Chen et al., SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens, J Med Virol
Pennings, Kritharides, CD147 in cardiovascular disease and thrombosis, Semin Thromb Hemost
Persson, Mccallum, Reiling, Lister, Stubbs et al., Variation in use of erythrocyte invasion pathways by Plasmodium falciparum mediates evasion of human inhibitory antibodies, J Clin Invest
Pillay, Gene of the month: the 2019-nCoV/SARS-CoV-2 novel coronavirus spike protein, Journal of Clinical Pathology
Popova, Zhang, The spike but not the hemagglutinin/esterase protein of bovine coronavirus is necessary and sufficient for viral infection, Virology
Pourrajab, Zare-Khormizi, Sheikhha, Molecular Basis for Pathogenicity of Human Coronaviruses, Infect Drug Resist
Price, Mccabe, Garfield, Wort, Thrombosis and COVID-19 pneumonia: the clot thickens!, European Respiratory Journal
Pryzdial, Lin, Sutherland, Virus-Platelet Associations
Pushkarsky, Zybarth, Dubrovsky, Yurchenko, Tang et al., CD147 facilitates HIV-1 infection by interacting with virus-associated cyclophilin A, Proc Natl Acad Sci
Qing, Hantak, Perlman, Gallagher, Distinct Roles for Sialoside and Protein Receptors in Coronavirus Infection, mBio
Radzikowska, Ding, Tan, Zhakparov, Peng et al., Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors, Allergy
Rajah, Bernier, Buchrieser, Schwartz, The Mechanism and Consequences of SARS-CoV-2 Spike-Mediated Fusion and Syncytia Formation, Journal of Molecular Biology,
doi:10.1016/j.jmb.2021.167280:167280Rapkiewicz, Mai, Carsons, Pittaluga, Kleiner et al., Megakaryocytes and plateletfibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series, EClinicalMedicine
Reid, Mohandas, Red blood cell blood group antigens: structure and function, Seminars in Hematology
Richardson, Schwartz, Comparison of capillary blood flow in the nailfold circulations of young and elderly men, AGE
Richardson, Shepherd, The cutaneous microcirculation of the forearm in young and old subjects, Microvascular Research
Robson, Bioinformatics studies on a function of the SARS-CoV-2 spike glycoprotein as the binding of host sialic acid glycans, Computers in Biology and Medicine
Roe, High COVID-19 virus replication rates, the creation of antigen-antibody immune complexes and indirect haemagglutination resulting in thrombosis, Transboundary and Emerging Diseases
Rowe, Claessens, Corrigan, Arman, Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications, Expert Reviews in Molecular Medicine
Rowe, Handel, Thera, Deans, Lyke et al., Blood group O protects against severe <em>Plasmodium falciparum</em> malaria through the mechanism of reduced rosetting, Proc Natl Acad Sci
Rowe, Opi, Williams, Blood groups and malaria: fresh insights into pathogenesis and identification of targets for intervention, Curr Opin Hematol
Ryu, Chapter 4 -Diagnosis and Methods
Sakariassen, Orning, Turitto, The impact of blood shear rate on arterial thrombus formation, Future Sci OA
Salk, A Plastic Plate for Use in Tests Involving Virus Hemagglutination and Other Similar Reactions, Science
Salk, A Simplified Procedure for Titrating Hemagglutinating Capacity of Influenza-Virus and the Corresponding Antibody, The Journal of Immunology
Sardu, Gambardella, Morelli, Wang, Marfella et al., Hypertension, Thrombosis, Kidney Failure, and Diabetes: Is COVID-19 an Endothelial Disease? A Comprehensive Evaluation of Clinical and Basic Evidence, J Clin Med
Sauter, Hanson, Glick, Brown, Crowther et al., Binding of influenza virus hemagglutinin to analogs of its cell-surface receptor, sialic acid: analysis by proton nuclear magnetic resonance spectroscopy and X-ray crystallography, Biochemistry
Scheim, A deadly embrace: Hemagglutination mediated by SARS-CoV-2 spike protein at its 22 Nglycosylation sites, red blood cell surface sialoglycoproteins, and antibody
Scheim, Ivermectin for COVID-19 treatment: clinical response at quasi-threshold doses via hypothesized alleviation of CD147-mediated vascular occlusion
Schmidt, Bültmann, Fischel, Gillitzer, Cullen et al., Extracellular matrix metalloproteinase inducer (CD147) is a novel receptor on platelets, activates platelets, and augments nuclear factor kappaBdependent inflammation in monocytes, Circ Res
Schultze, Cavanagh, Herrler, Neuraminidase treatment of avian infectious bronchitis coronavirus reveals a hemagglutinating activity that is dependent on sialic acid-containing receptors on erythrocytes, Virology
Schultze, Gross, Brossmer, Klenk, Herrler, Hemagglutinating encephalomyelitis virus attaches to N-acetyl-9-O-acetylneuraminic acid-containing receptors on erythrocytes: comparison with bovine coronavirus and influenza C virus, Virus Res
Schulz, Brühl, Barocke, Cullen, Mayer et al., EMMPRIN (CD147/basigin) mediates platelet-monocyte interactions in vivo and augments monocyte recruitment to the vascular wall, J Thromb Haemost
Schwegmann-Wessels, Herrler, Sialic acids as receptor determinants for coronaviruses, Glycoconj J
Seizer, Ungern-Sternberg, Schönberger, Borst, Münzer et al., Extracellular cyclophilin A activates platelets via EMMPRIN (CD147) and PI3K/Akt signaling, which promotes platelet adhesion and thrombus formation in vitro and in vivo, Arterioscler Thromb Vasc Biol
Shahid, Nunhuck, Physiology
Shajahan, Supekar, Gleinich, Azadi, Deducing the N-and O-glycosylation profile of the spike protein of novel coronavirus SARS-CoV-2, Glycobiology
Sharma, Rawat, Janakiraman, Gromiha, Elucidating important structural features for the binding affinity of spike -SARS-CoV-2 neutralizing antibody complexes, Proteins: Structure, Function, and Bioinformatics
Shelokov, Vogel, Hemadsorption (Adsorption-Hemagglutination) Test for Viral Agents in Tissue Culture with Special Reference to Influenza, Proc Soc Exp Biol Med
Sieben, Kappel, Zhu, Wozniak, Rankl et al., Influenza virus binds its host cell using multiple dynamic interactions, Proc Natl Acad Sci
Silva-Filho, Cgfd, Jld, The influence of ABO blood groups on COVID-19 susceptibility and severity: A molecular hypothesis based on carbohydrate-carbohydrate interactions, Medical Hypotheses
Smith, Tusell, Travanty, Berkhout, Van Der Hoek et al., Human angiotensin-converting enzyme 2 (ACE2) is a receptor for human respiratory coronavirus NL63, Adv Exp Med Biol
Soerensen, Wandall, Patel, Richardson, Italiano et al., Platelets Lacking Sialic Acid Clear Rapidly from the Circulation Due to Ingestion by Asialoglycoprotein Receptor-Expressing Liver Macrophages and Hepatocytes, Blood
Sriwilaijaroen, Suzuki, Sialoglycovirology of Lectins: Sialyl Glycan Binding of Enveloped and Nonenveloped Viruses
Stocker, Ishikawa-Ankerhold, Massberg, Schulz, Small but mighty: Platelets as central effectors of host defense, Thromb Haemost
Storry, Review: the function of blood group-specific RBC membrane components, Immunohematology
Storz, Zhang, Rott, Comparison of hemagglutinating, receptor-destroying, and acetylesterase activities of avirulent and virulent bovine coronavirus strains, Archives of Virology
Ströh, Stehle, Glycan Engagement by Viruses: Receptor Switches and Specificity, Annu Rev Virol
Su, Yang, Wan, Yi, Tang et al., Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China, Kidney International
Sugiyama, Kasai, Kato, Kasai, Hatakeyama, Haemagglutinin-esterase protein (HE) of murine corona virus: DVIM (diarrhea virus of infant mice), Arch Virol
Szczepanski, Owczarek, Bzowska, Gula, Drebot et al., Canine Respiratory Coronavirus, Bovine Coronavirus, and Human Coronavirus OC43: Receptors and Attachment Factors, Viruses
Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, Journal of Thrombosis and Haemostasis
Taoufiq, Gay, Balvanyos, Ciceron, Tefit et al., Rho Kinase Inhibition in Severe Malaria: Thwarting Parasite-Induced Collateral Damage to Endothelia, The Journal of Infectious Diseases
Taube, Perry, Yetming, Patel, Auble et al., Ganglioside-Linked Terminal Sialic Acid Moieties on Murine Macrophages Function as Attachment Receptors for Murine Noroviruses, J Virol
Thompson, De Vries, Paulson, Virus recognition of glycan receptors, Current Opinion in Virology
Tiralongo, Chapter 29 -Sialic acid-specific microbial lectins
Tiwari, Beer, Sankaranarayanan, Swanson-Mungerson, Desai, Discovering small-molecule therapeutics against SARS-CoV-2, Drug Discovery Today
Tortorici, Veesler, Chapter Four -Structural insights into coronavirus entry, Advances in Virus Research
Tortorici, Walls, Lang, Wang, Li et al., Structural basis for human coronavirus attachment to sialic acid receptors, Nat Struct Mol Biol
Tsuchida, The effect of aging and arteriosclerosis on human skin blood flow, J Dermatol Sci
Valyaeva, Zharikova, Kasianov, Vassetzky, Sheval, Expression of SARS-CoV-2 entry factors in lung epithelial stem cells and its potential implications for COVID-19, Scientific Reports
Vanarsdall, Pritchard, Wisner, Liu, Jardetzky et al., CD147 Promotes Entry of Pentamer-Expressing Human Cytomegalovirus into Epithelial and Endothelial Cells, mBio
Varki, Gagneux, Multifarious roles of sialic acids in immunity, Ann N Y Acad Sci
Vbdbd, Lednicky, White, Loeb, Elbadry et al., Isolation of Coronavirus NL63 from Blood from Children in Rural Haiti: Phylogenetic Similarities with Recent Isolates from Malaysia, Am J Trop Med Hyg
Veyer, Kernéis, Poulet, Wack, Robillard et al., Highly sensitive quantification of plasma SARS-CoV-2 RNA shelds light on its potential clinical value, Clin Infect Dis,
doi:10.1093/cid/ciaa1196.206Vigan-Womas, Guillotte, Juillerat, Hessel, Raynal et al., Structural basis for the ABO blood-group dependence of Plasmodium falciparum rosetting, PLoS Pathog
Vlasak, Luytjes, Spaan, Palese, Human and bovine coronaviruses recognize sialic acid-containing receptors similar to those of influenza C viruses, Proc Natl Acad Sci
Von Ungern-Sternberg, Zernecke, Seizer, Extracellular Matrix Metalloproteinase Inducer EMMPRIN (CD147) in Cardiovascular Disease, International Journal of Molecular Sciences
Wagner, Matrosovich, Klenk, Functional balance between haemagglutinin and neuraminidase in influenza virus infections, Rev Med Virol
Walls, Tortorici, Frenz, Snijder, Li et al., Glycan shield and epitope masking of a coronavirus spike protein observed by cryo-electron microscopy, Nat Struct Mol Biol
Wang, Chen, Zhang, Deng, Lian et al., CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells, Signal Transduction and Targeted Therapy
Wang, Saguner, An, Ning, Yan et al., Dysfunctional Coagulation in COVID-19: From Cell to Bedside, Advances in Therapy
Wang, Zhang, Wu, Niu, Song et al., Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2, Cell
Wassmer, Grau, Severe malaria: what's new on the pathogenesis front?, Int J Parasitol
Watanabe, Allen, Wrapp, Mclellan, Crispin, Site-specific glycan analysis of the SARS-CoV-2 spike, Science
Wibmer, Ayres, Hermanus, Madzivhandila, Kgagudi et al., SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma, Nat Med
Wielgat, Rogowski, Godlewska, Car, Coronaviruses: Is Sialic Acid a Gate to the Eye of Cytokine Storm? From the Entry to the Effects, Cells
Williamson, Walker, Bhaskaran, Bacon, Bates et al., OpenSAFELY: factors associated with COVID-19 death in 17 million patients, Nature
Wölfel, Corman, Guggemos, Seilmaier, Zange et al., Virological assessment of hospitalized patients with COVID-2019, Nature
Xiong, Coombs, Martin, Liu, Xiao et al., Receptor binding by a ferret-transmissible H5 avian influenza virus, Nature
Xiong, Tortorici, Snijder, Yoshioka, Walls et al., Glycan Shield and Fusion Activation of a Deltacoronavirus Spike Glycoprotein Fine-Tuned for Enteric Infections, J Virol
Xu, David, A Simple Model of Multivalent Adhesion and Its Application to Influenza Infection, Biophysical Journal
Yagisawa, Foster, Hanaki, Omura, Campbell, History of avermectin and ivermectin, with notes on the history of other macrocyclic lactone antiparasitic agents, The Japanese Journal of Antibiotics
Yee, Main, Terry, Stevanovski, Maczurek et al., CD147 mediates intrahepatic leukocyte aggregation and determines the extent of liver injury, PLoS One
Yoshimoto, The Proteins of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2 or n-COV19), the Cause of COVID-19, The Protein Journal
Yurchenko, Constant, Bukrinsky, Dealing with the family: CD147 interactions with cyclophilins, Immunology
Zaki, Van Boheemen, Bestebroer, Osterhaus, Fouchier, Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia, N Engl J Med
Zeng, Langereis, Van Vliet, Huizinga, De Groot, Structure of coronavirus hemagglutininesterase offers insight into corona and influenza virus evolution, Proc Natl Acad Sci
Zenonos, Dummler, Müller-Sienerth, Chen, Preiser et al., Basigin is a druggable target for host-oriented antimalarial interventions, J Exp Med
Zhang, Du, Li, Zheng, Yang et al., Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes, Emerg Microbes Infect
Zheng, Yu, Feng, Lou, Zou, Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study, BMJ
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhu, Song, Zhang, Nanda, Li, CD147: A Novel Modulator of Inflammatory and Immune Disorders, Current Medicinal Chemistry
Zietz, Zucker, Tatonetti, Associations between blood type and COVID-19 infection, intubation, and death, Nat Commun
DOI record:
{
"DOI": "10.31219/osf.io/sgdj2",
"URL": "http://dx.doi.org/10.31219/osf.io/sgdj2",
"abstract": "<p>The role of vascular occlusion in the morbidities, pulmonary and systemic, of COVID-19 has received increasing focus. Histological studies of lung tissue from COVID-19 patients have found extensively damaged endothelium of capillaries adjoining relatively intact alveoli, corresponding to hypoxemia accompanying normal breathing mechanics in such patients.Essential to the study of vascular occlusion in COVID-19 are viral properties dating back to studies of Jonas Salk in the 1940s that have been positively established for SARS-CoV-2. First, SARS-CoV-2 binds to red blood cells (RBCs) in vitro and also clinically in COVID-19 patients. Second, although fusion and replication of SARS-CoV-2 occur via ACE2, such hemagglutinating viruses initially attach to infective targets and clump with blood cells via much more abundantly distributed glycoconjugate binding sites, notably those tipped with sialic acid (SA). SARS-CoV-2, in particular, attaches to these glycan binding sites. Third, certain enveloped viruses express an enzyme, hemagglutinin esterase (HE), that counteracts viral-RBC clumping. Notably, among betacoronaviruses, the common cold strains express HE while SARS-CoV-2, SARS-CoV-1 and MERS, the virulent strains, do not. The hemagglutinating properties of SARS-COV-2 establish a framework for “catch and clump” induction of microvascular occlusion proposed here. Ultramicroscopic studies of tissues from COVID-19 patients indicate a key role for hemagglutination early and mid-course in COVID-19, before such clumps develop into clots via the coagulation cascade.</p>",
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6841-7054",
"affiliation": [],
"authenticated-orcid": true,
"family": "Scheim",
"given": "David",
"sequence": "first"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
10,
18
]
],
"date-time": "2022-10-18T05:00:57Z",
"timestamp": 1666069257000
},
"deposited": {
"date-parts": [
[
2022,
10,
18
]
],
"date-time": "2022-10-18T05:00:59Z",
"timestamp": 1666069259000
},
"group-title": "Open Science Framework",
"indexed": {
"date-parts": [
[
2023,
12,
1
]
],
"date-time": "2023-12-01T14:17:53Z",
"timestamp": 1701440273218
},
"is-referenced-by-count": 4,
"issued": {
"date-parts": [
[
2022,
10,
17
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/legalcode",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
17
]
],
"date-time": "2022-10-17T00:00:00Z",
"timestamp": 1665964800000
}
}
],
"member": "15934",
"original-title": [],
"posted": {
"date-parts": [
[
2022,
10,
17
]
]
},
"prefix": "10.31219",
"published": {
"date-parts": [
[
2022,
10,
17
]
]
},
"publisher": "Center for Open Science",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://osf.io/sgdj2"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells",
"type": "posted-content"
}