Ivermectin and mortality in patients with COVID-19: A systematic review, meta-analysis, and meta-regression of randomized controlled trials
Ahmad Fariz Malvi Zamzam Zein, Catur Setiya Sulistiyana, Wilson Matthew Raffaelo, Raymond Pranata
Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2021.102186
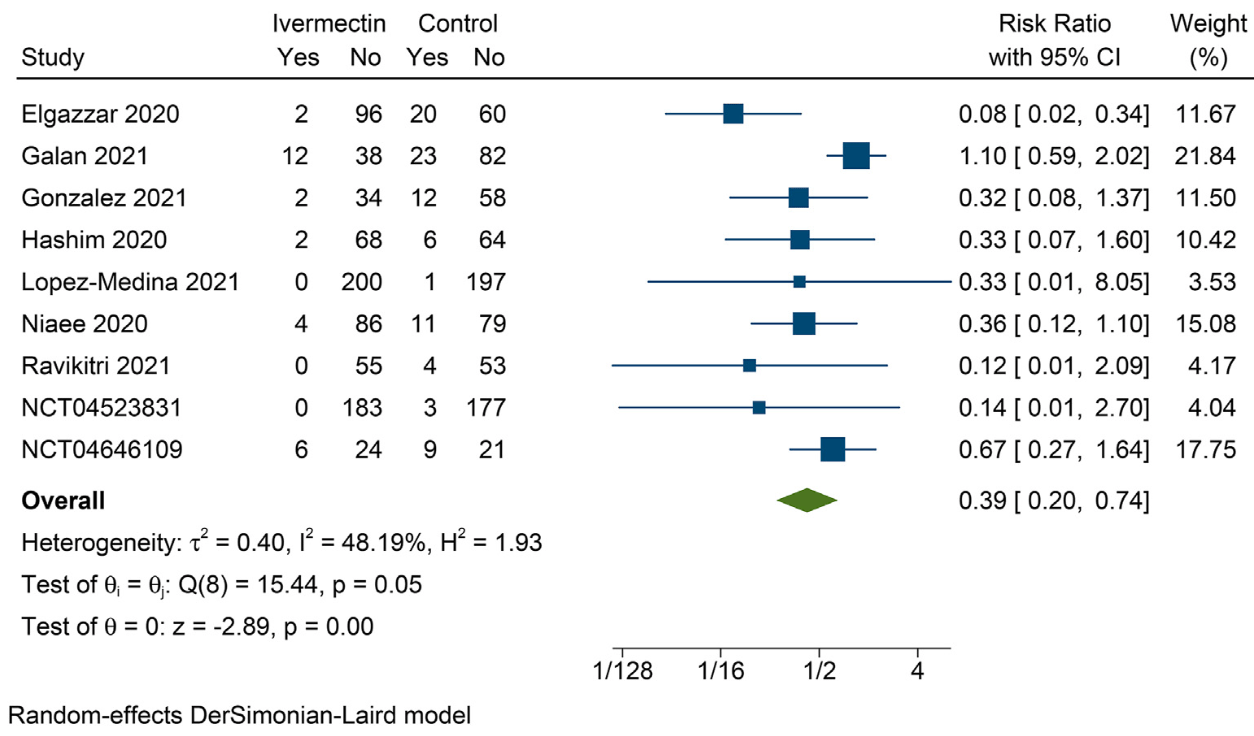
Aims: This systematic review and meta-analysis aims to investigate the effect of ivermectin on mortality in patients with COVID-19. Methods: A comprehensive systematic literature search was performed using PubMed, Scopus, Embase, and Clinicaltrials.gov from the inception of databases up until April 9, 2021. The intervention group was ivermectin and the control group was standard of care or placebo. The primary outcome was mortality reported as risk ratio (RR). Results: There were 9 RCTs comprising of 1788 patients included in this meta-analysis. Ivermectin was associated with decreased mortality (RR 0.39 [95% 0.20e0.74], p ¼ 0.004; I 2 : 58.2%, p ¼ 0.051). Subgroup analysis in patients with severe COVID-19 showed borderline statistical significance towards mortality reduction (RR 0.42 [95% 0.18e1.00], p ¼ 0.052; I 2 : 68.3, p ¼ 0.013). The benefit of ivermectin and mortality was reduced by hypertension (RR 1.08 [95% CI 1.03e1.13], p ¼ 0.001); but was not influenced by age (p ¼ 0.657), sex (p ¼ 0.466), diabetes (p ¼ 0.429). Sensitivity analysis using fixed-effect model showed that ivermectin decreased mortality in general (RR 0.43 [95% CI 0.29e0.62], p < 0.001) and severe COVID-19 subgroup (RR 0.48 [95% CI 0.32e0.72], p < 0.001). Conclusions: Ivermectin was associated with decreased mortality in COVID-19 with a low certainty of evidence. Further adequately powered double-blinded placebo-controlled RCTs are required for definite conclusion.
References
Ashraf, Chaudhry, Raza, Ghosh, Zhao, In vitro activity of ivermectin against Staphylococcus aureus clinical isolates, Antimicrob Resist Infect Contr,
doi:10.1186/s13756-018-0314-4Barrows, Campos, Powell, Prasanth, Schott-Lerner et al., A screen of FDA-approved drugs for inhibitors of zika virus infection, Cell Host Microbe,
doi:10.1016/j.chom.2016.07.004Canga, Prieto, Li Ebana, Martínez, Vega et al., The pharmacokinetics and interactions of ivermectin in humans -a mini-review, AAPS J,
doi:10.1208/s12248-007-9000-9Crump, Ivermectin: enigmatic multifaceted "wonder" drug continues to surprise and exceed expectations, J Antibiot (Tokyo),
doi:10.1038/ja.2017.11Elgazzar, Eltaweel, Youssef, Hany, Hafez, Efficacy and safety of ivermectin for treatment and prophylaxis of COVID-19 pandemic, Res Sq,
doi:10.21203/rs.3.rs-100956/v3Galan, Santos Nm Dos, Asato, Araújo, De Lima Moreira et al., Phase 2 randomized study on chloroquine, hydroxychloroquine or ivermectin in hospitalized patients with severe manifestations of SARS-CoV-2 infection, Pathog Glob Health,
doi:10.1080/20477724.2021.1890887Gonzalez, Gonz Alez G Amez, Enciso, Maldonado, Efficacy and safety of Ivermectin and Hydroxychloroquine in patients with severe COVID-19. A randomized controlled trial Corresponding Authors, MedRxiv,
doi:10.1101/2021.02.18.21252037G€ Otz, Magar, Dornfeld, Giese, Pohlmann et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Sci Rep,
doi:10.1038/srep23138Handayani, Juliastuti, Nawangsih, Kusmala, Rakhmat et al., Prognostic value of fasting hyperglycemia in patients with COVID-19 e diagnostic test accuracy meta-analysis, Obes Med,
doi:10.1016/j.obmed.2021.100333Hashim, Maulood, Rasheed, Fatak, Kabah et al., Controlled randomized clinical trial on using Ivermectin with Doxycycline for treating COVID-19 patients in Baghdad, Iraq. MedRxiv,
doi:10.1101/2020.10.26.20219345Huang, Pranata, Lim, Oehadian, Alisjahbana, C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis, Ther Adv Respir Dis,
doi:10.1177/1753466620937175Intuyod, Hahnvajanawong, Pinlaor, Pinlaor, Anti-parasitic drug ivermectin exhibits potent anticancer activity against gemcitabine-resistant cholangiocarcinoma in vitro, Anticancer Res,
doi:10.21873/anticanres.13669Juarez, Schcolnik-Cabrera, Dueñas-Gonzalez, The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug, Am J Cancer Res
Klotz, Ogbuokiri, Okonkwo, Ivermectin binds avidly to plasma proteins, Eur J Clin Pharmacol,
doi:10.1007/BF00316107Lim, Pranata, Huang, Yonas, Soeroto et al., Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis, Can J Kidney Heal Dis,
doi:10.1177/2054358120938573Lim, Vilch Eze, Ng, Jacobs, On-García et al., Anthelmintic avermectins kill mycobacterium tuberculosis, including multidrugresistant clinical strains, Antimicrob Agents Chemother,
doi:10.1128/AAC.01696-12Lukito, Pranata, Henrina, Lim, Lawrensia et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev,
doi:10.1016/j.dsx.2020.11.006Martha, Pranata, Lim, Wibowo, Akbar, Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates, Int J Infect Dis,
doi:10.1016/j.ijid.2021.05.016Niaee, Gheibi, Namdar, Allami, Zolghadr et al., Ivermectin as an adjunct treatment for hospitalized adult COVID-19 patients: a randomized multi-center clinical trial, Res Sq,
doi:10.21203/rs.3.rs-109670/v1Opez-Medina, Hurtado, Ramirez, Martínez, Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial, JAMA, J Am Med Assoc,
doi:10.1001/jama.2021.3071Portmann-Baracco, Alberti, Accinelli, Antiviral and antiinflammatory properties of ivermectin and its potential use in COVID-19, Arch Bronconeumol,
doi:10.1016/j.arbres.2020.06.011Pranata, Huang, Lim, Yonas, Vania et al., Delirium and mortality in coronavirus disease 2019 (COVID-19) e a systematic review and meta-analysis, Arch Gerontol Geriatr,
doi:10.1016/j.archger.2021.104388Pranata, Huang, Raharjo, Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis, Indian Pacing Electrophysiol J,
doi:10.1016/j.ipej.2020.08.001Pranata, Lim, Huang, Raharjo, Lukito, Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression, JRAAS -J Renin-Angiotensin-Aldosterone Syst,
doi:10.1177/1470320320926899Pranata, Permana, Huang, Lim, Soetedjo et al., The use of renin angiotensin system inhibitor on mortality in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev,
doi:10.1016/j.dsx.2020.06.047Rajter, Sherman, Fatteh, Vogel, Sacks et al., Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ivermectin in COVID nineteen study, Chest,
doi:10.1016/j.chest.2020.10.009Rakhmat, Kusmala, Handayani, Juliastuti, Nawangsih et al., Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19) e a systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr Clin Res Rev,
doi:10.1016/j.dsx.2021.03.027Roy, Pattadar, Raj, Agarwal, Biswas, Ivermectin as a potential treatment for mild to moderate COVID-19 e a double blind randomized placebo-controlled trial, MedRxiv,
doi:10.1101/2021.01.05.21249310Sharun, Dhama, Patel, Pathak, Tiwari et al., Ivermectin, a new candidate therapeutic against SARS-CoV-2/COVID-19, Ann Clin Microbiol Antimicrob,
doi:10.1186/s12941-020-00368-wTay, Fraser, Chan, Moreland, Rathore et al., Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antivir Res,
doi:10.1016/j.antiviral.2013.06.002Ventre, Rozi Eres, Lenief, Albert, Rossio et al., Topical ivermectin improves allergic skin inflammation, Allergy Eur J Allergy Clin Immunol,
doi:10.1111/all.13118Wagstaff, Sivakumaran, Heaton, Harrich, Jans, Ivermectin is a specific inhibitor of importin a/b-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochem J,
doi:10.1042/BJ20120150Who, Weekly epidemiological update -2
Yan, Ci, Chen, Chen, Li et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflamm Res,
doi:10.1007/s00011-011-0307-8Yang, Atkinson, Wang, Lee, Bogoyevitch et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin a/b1 heterodimer, Antivir Res,
doi:10.1016/j.antiviral.2020.104760Yonas, Alwi, Pranata, Huang, Lim et al., Elevated interleukin levels are associated with higher severity and mortality in COVID 19 e a systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr Clin Res Rev,
doi:10.1016/j.dsx.2020.11.011Zhang, Song, Ci, Ju, Li, Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflamm Res,
doi:10.1007/s00011-008-8007-8DOI record:
{
"DOI": "10.1016/j.dsx.2021.102186",
"ISSN": [
"1871-4021"
],
"URL": "http://dx.doi.org/10.1016/j.dsx.2021.102186",
"alternative-id": [
"S187140212100206X"
],
"article-number": "102186",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Ivermectin and mortality in patients with COVID-19: A systematic review, meta-analysis, and meta-regression of randomized controlled trials"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.dsx.2021.102186"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Diabetes India. Published by Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7821-3813",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zein",
"given": "Ahmad Fariz Malvi Zamzam",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7574-7745",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sulistiyana",
"given": "Catur Setiya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Raffaelo",
"given": "Wilson Matthew",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3998-6551",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pranata",
"given": "Raymond",
"sequence": "additional"
}
],
"container-title": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews",
"container-title-short": "Diabetes & Metabolic Syndrome: Clinical Research & Reviews",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
6,
27
]
],
"date-time": "2021-06-27T13:48:15Z",
"timestamp": 1624801695000
},
"deposited": {
"date-parts": [
[
2022,
1,
10
]
],
"date-time": "2022-01-10T17:41:12Z",
"timestamp": 1641836472000
},
"indexed": {
"date-parts": [
[
2023,
3,
31
]
],
"date-time": "2023-03-31T17:27:12Z",
"timestamp": 1680283632309
},
"is-referenced-by-count": 21,
"issue": "4",
"issued": {
"date-parts": [
[
2021,
7
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
1
]
],
"date-time": "2021-07-01T00:00:00Z",
"timestamp": 1625097600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S187140212100206X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S187140212100206X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "102186",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
7
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"author": "Who",
"key": "10.1016/j.dsx.2021.102186_bib1",
"series-title": "Weekly epidemiological update - 2 March 2021",
"year": "2021"
},
{
"DOI": "10.1016/j.ipej.2020.08.001",
"article-title": "Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis",
"author": "Pranata",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Indian Pacing Electrophysiol J",
"key": "10.1016/j.dsx.2021.102186_bib2",
"volume": "20",
"year": "2020"
},
{
"article-title": "Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis",
"author": "Lim",
"journal-title": "Can J Kidney Heal Dis",
"key": "10.1016/j.dsx.2021.102186_bib3",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.archger.2021.104388",
"article-title": "Delirium and mortality in coronavirus disease 2019 (COVID-19) – a systematic review and meta-analysis",
"author": "Pranata",
"doi-asserted-by": "crossref",
"first-page": "104388",
"journal-title": "Arch Gerontol Geriatr",
"key": "10.1016/j.dsx.2021.102186_bib4",
"volume": "95",
"year": "2021"
},
{
"DOI": "10.1177/1753466620937175",
"article-title": "C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis",
"author": "Huang",
"doi-asserted-by": "crossref",
"journal-title": "Ther Adv Respir Dis",
"key": "10.1016/j.dsx.2021.102186_bib5",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.11.011",
"article-title": "Elevated interleukin levels are associated with higher severity and mortality in COVID 19 – a systematic review, meta-analysis, and meta-regression",
"author": "Yonas",
"doi-asserted-by": "crossref",
"first-page": "2219",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.dsx.2021.102186_bib6",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s00210-020-01902-5",
"article-title": "Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action",
"author": "Rizzo",
"doi-asserted-by": "crossref",
"first-page": "1153",
"journal-title": "Naunyn-Schmiedeberg’s Arch Pharmacol",
"key": "10.1016/j.dsx.2021.102186_bib7",
"volume": "393",
"year": "2020"
},
{
"DOI": "10.1208/s12248-007-9000-9",
"article-title": "The pharmacokinetics and interactions of ivermectin in humans - a mini-review",
"author": "Canga",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "AAPS J",
"key": "10.1016/j.dsx.2021.102186_bib8",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1128/AAC.01696-12",
"article-title": "Anthelmintic avermectins kill mycobacterium tuberculosis, including multidrug-resistant clinical strains",
"author": "Lim",
"doi-asserted-by": "crossref",
"first-page": "1040",
"journal-title": "Antimicrob Agents Chemother",
"key": "10.1016/j.dsx.2021.102186_bib9",
"volume": "57",
"year": "2013"
},
{
"article-title": "In vitro activity of ivermectin against Staphylococcus aureus clinical isolates",
"author": "Ashraf",
"journal-title": "Antimicrob Resist Infect Contr",
"key": "10.1016/j.dsx.2021.102186_bib10",
"volume": "7",
"year": "2018"
},
{
"article-title": "The multitargeted drug ivermectin: from an antiparasitic agent to a repositioned cancer drug",
"author": "Juarez",
"first-page": "317",
"journal-title": "Am J Cancer Res",
"key": "10.1016/j.dsx.2021.102186_bib11",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.21873/anticanres.13669",
"article-title": "Anti-parasitic drug ivermectin exhibits potent anticancer activity against gemcitabine-resistant cholangiocarcinoma in vitro",
"author": "Intuyod",
"doi-asserted-by": "crossref",
"first-page": "4837",
"journal-title": "Anticancer Res",
"key": "10.1016/j.dsx.2021.102186_bib12",
"volume": "39",
"year": "2019"
},
{
"DOI": "10.1016/j.vetpar.2016.06.015",
"article-title": "Ivermectin exhibits potent anti-mitotic activity",
"author": "Ashraf",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Vet Parasitol",
"key": "10.1016/j.dsx.2021.102186_bib13",
"volume": "226",
"year": "2016"
},
{
"DOI": "10.1111/all.13118",
"article-title": "Topical ivermectin improves allergic skin inflammation",
"author": "Ventre",
"doi-asserted-by": "crossref",
"first-page": "1212",
"journal-title": "Allergy Eur J Allergy Clin Immunol",
"key": "10.1016/j.dsx.2021.102186_bib14",
"volume": "72",
"year": "2017"
},
{
"DOI": "10.1016/j.antiviral.2012.06.008",
"article-title": "Nuclear trafficking of proteins from RNA viruses: potential target for antivirals?",
"author": "Caly",
"doi-asserted-by": "crossref",
"first-page": "202",
"journal-title": "Antivir Res",
"key": "10.1016/j.dsx.2021.102186_bib15",
"volume": "95",
"year": "2012"
},
{
"DOI": "10.1016/j.antiviral.2013.06.002",
"article-title": "Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "Antivir Res",
"key": "10.1016/j.dsx.2021.102186_bib16",
"volume": "99",
"year": "2013"
},
{
"DOI": "10.1016/j.antiviral.2020.104760",
"article-title": "The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer",
"author": "Yang",
"doi-asserted-by": "crossref",
"journal-title": "Antivir Res",
"key": "10.1016/j.dsx.2021.102186_bib17",
"volume": "177",
"year": "2020"
},
{
"article-title": "Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import",
"author": "Götz",
"journal-title": "Sci Rep",
"key": "10.1016/j.dsx.2021.102186_bib18",
"volume": "6",
"year": "2016"
},
{
"article-title": "Controlled randomized clinical trial on using Ivermectin with Doxycycline for treating COVID-19 patients in Baghdad, Iraq",
"author": "Hashim",
"journal-title": "MedRxiv",
"key": "10.1016/j.dsx.2021.102186_bib19",
"volume": "48",
"year": "2020"
},
{
"article-title": "Ivermectin as an adjunct treatment for hospitalized adult COVID-19 patients: a randomized multi-center clinical trial",
"author": "Niaee",
"journal-title": "Res Sq",
"key": "10.1016/j.dsx.2021.102186_bib20",
"year": "2020"
},
{
"DOI": "10.1016/j.chest.2020.10.009",
"article-title": "Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ivermectin in COVID nineteen study",
"author": "Rajter",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Chest",
"key": "10.1016/j.dsx.2021.102186_bib21",
"volume": "159",
"year": "2021"
},
{
"article-title": "Ivermectin as a potential treatment for mild to moderate COVID-19 – a double blind randomized placebo-controlled trial",
"author": "Ravikirti",
"journal-title": "MedRxiv 2021",
"key": "10.1016/j.dsx.2021.102186_bib22",
"year": "2021"
},
{
"article-title": "Efficacy and safety of ivermectin for treatment and prophylaxis of COVID-19 pandemic",
"author": "Elgazzar",
"journal-title": "Res Sq",
"key": "10.1016/j.dsx.2021.102186_bib23",
"year": "2020"
},
{
"article-title": "Phase 2 randomized study on chloroquine, hydroxychloroquine or ivermectin in hospitalized patients with severe manifestations of SARS-CoV-2 infection",
"author": "Galan",
"first-page": "1",
"journal-title": "Pathog Glob Health",
"key": "10.1016/j.dsx.2021.102186_bib24",
"year": "2021"
},
{
"article-title": "Efficacy and safety of Ivermectin and Hydroxychloroquine in patients with severe COVID-19. A randomized controlled trial Corresponding Authors",
"author": "Gonzalez",
"journal-title": "MedRxiv 2021",
"key": "10.1016/j.dsx.2021.102186_bib25",
"year": "2021"
},
{
"key": "10.1016/j.dsx.2021.102186_bib26",
"unstructured": "Ivermectin for severe COVID-19 Management - NCT04646109- ClinicalTrials.[gov n.d]."
},
{
"key": "10.1016/j.dsx.2021.102186_bib27",
"unstructured": "Clinical trial of ivermectin Plus Doxycycline for the treatment of Confirmed Covid-19 infection - NCT04523831 - ClinicalTrials.[gov n.d]."
},
{
"DOI": "10.1001/jama.2021.3071",
"article-title": "Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial",
"author": "López-Medina",
"doi-asserted-by": "crossref",
"first-page": "1426",
"journal-title": "JAMA, J Am Med Assoc",
"key": "10.1016/j.dsx.2021.102186_bib28",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.06.047",
"article-title": "The use of renin angiotensin system inhibitor on mortality in patients with coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis",
"author": "Pranata",
"doi-asserted-by": "crossref",
"first-page": "983",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.dsx.2021.102186_bib29",
"volume": "14",
"year": "2020"
},
{
"article-title": "Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: a systematic review, meta-analysis and meta-regression",
"author": "Pranata",
"journal-title": "JRAAS - J Renin-Angiotensin-Aldosterone Syst",
"key": "10.1016/j.dsx.2021.102186_bib30",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1016/j.obmed.2021.100333",
"article-title": "Prognostic value of fasting hyperglycemia in patients with COVID-19 – diagnostic test accuracy meta-analysis",
"author": "Handayani",
"doi-asserted-by": "crossref",
"first-page": "100333",
"journal-title": "Obes Med",
"key": "10.1016/j.dsx.2021.102186_bib31",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "Lukito",
"doi-asserted-by": "crossref",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.dsx.2021.102186_bib32",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2021.03.027",
"article-title": "Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19) – a systematic review, meta-analysis, and meta-regression",
"author": "Rakhmat",
"doi-asserted-by": "crossref",
"first-page": "777",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "10.1016/j.dsx.2021.102186_bib33",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.metabol.2021.154814",
"article-title": "Diabetes and COVID-19: the past, the present, and the future",
"author": "Pranata",
"doi-asserted-by": "crossref",
"first-page": "154814",
"journal-title": "Metabolism",
"key": "10.1016/j.dsx.2021.102186_bib34",
"year": "2021"
},
{
"DOI": "10.1042/BJ20120150",
"article-title": "Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus",
"author": "Wagstaff",
"doi-asserted-by": "crossref",
"first-page": "851",
"journal-title": "Biochem J",
"key": "10.1016/j.dsx.2021.102186_bib35",
"volume": "443",
"year": "2012"
},
{
"DOI": "10.1016/j.chom.2016.07.004",
"article-title": "A screen of FDA-approved drugs for inhibitors of zika virus infection",
"author": "Barrows",
"doi-asserted-by": "crossref",
"first-page": "259",
"journal-title": "Cell Host Microbe",
"key": "10.1016/j.dsx.2021.102186_bib36",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.1038/ja.2017.11",
"article-title": "Ivermectin: enigmatic multifaceted “wonder” drug continues to surprise and exceed expectations",
"author": "Crump",
"doi-asserted-by": "crossref",
"first-page": "495",
"journal-title": "J Antibiot (Tokyo)",
"key": "10.1016/j.dsx.2021.102186_bib37",
"volume": "70",
"year": "2017"
},
{
"DOI": "10.1007/BF00316107",
"article-title": "Ivermectin binds avidly to plasma proteins",
"author": "Klotz",
"doi-asserted-by": "crossref",
"first-page": "607",
"journal-title": "Eur J Clin Pharmacol",
"key": "10.1016/j.dsx.2021.102186_bib38",
"volume": "39",
"year": "1990"
},
{
"DOI": "10.1016/S0006-3495(03)74455-5",
"article-title": "Osmotic shock and the strength of viral capsids",
"author": "Cordova",
"doi-asserted-by": "crossref",
"first-page": "70",
"journal-title": "Biophys J",
"key": "10.1016/j.dsx.2021.102186_bib39",
"volume": "85",
"year": "2003"
},
{
"DOI": "10.1016/j.antiviral.2020.104759",
"article-title": "A potential role for integrins in host cell entry by SARS-CoV-2",
"author": "Sigrist",
"doi-asserted-by": "crossref",
"journal-title": "Antivir Res",
"key": "10.1016/j.dsx.2021.102186_bib40",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.1007/s00011-008-8007-8",
"article-title": "Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "524",
"journal-title": "Inflamm Res",
"key": "10.1016/j.dsx.2021.102186_bib41",
"volume": "57",
"year": "2008"
},
{
"DOI": "10.1007/s00011-011-0307-8",
"article-title": "Anti-inflammatory effects of ivermectin in mouse model of allergic asthma",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "589",
"journal-title": "Inflamm Res",
"key": "10.1016/j.dsx.2021.102186_bib42",
"volume": "60",
"year": "2011"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly",
"doi-asserted-by": "crossref",
"journal-title": "Antivir Res",
"key": "10.1016/j.dsx.2021.102186_bib43",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1016/j.arbres.2020.06.011",
"article-title": "Antiviral and anti-inflammatory properties of ivermectin and its potential use in COVID-19",
"author": "Portmann-Baracco",
"doi-asserted-by": "crossref",
"first-page": "831",
"journal-title": "Arch Bronconeumol",
"key": "10.1016/j.dsx.2021.102186_bib44",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.1186/s12941-020-00368-w",
"article-title": "Ivermectin, a new candidate therapeutic against SARS-CoV-2/COVID-19",
"author": "Sharun",
"doi-asserted-by": "crossref",
"journal-title": "Ann Clin Microbiol Antimicrob",
"key": "10.1016/j.dsx.2021.102186_bib45",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2021.05.016",
"article-title": "Active prescription of low-dose aspirin during or prior to hospitalization and mortality in COVID-19: a systematic review and meta-analysis of adjusted effect estimates",
"author": "Martha",
"doi-asserted-by": "crossref",
"first-page": "6",
"journal-title": "Int J Infect Dis",
"key": "10.1016/j.dsx.2021.102186_bib46",
"volume": "108",
"year": "2021"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S187140212100206X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Ivermectin and mortality in patients with COVID-19: A systematic review, meta-analysis, and meta-regression of randomized controlled trials",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "15"
}