Clinical Disease Characteristics and Treatment Trajectories Associated with Mortality among COVID-19 Patients in Punjab, Pakistan
Muhammad Zeeshan Munir, Amer Hayat Khan, Tahir Mehmood Khan
doi:10.3390/healthcare11081192
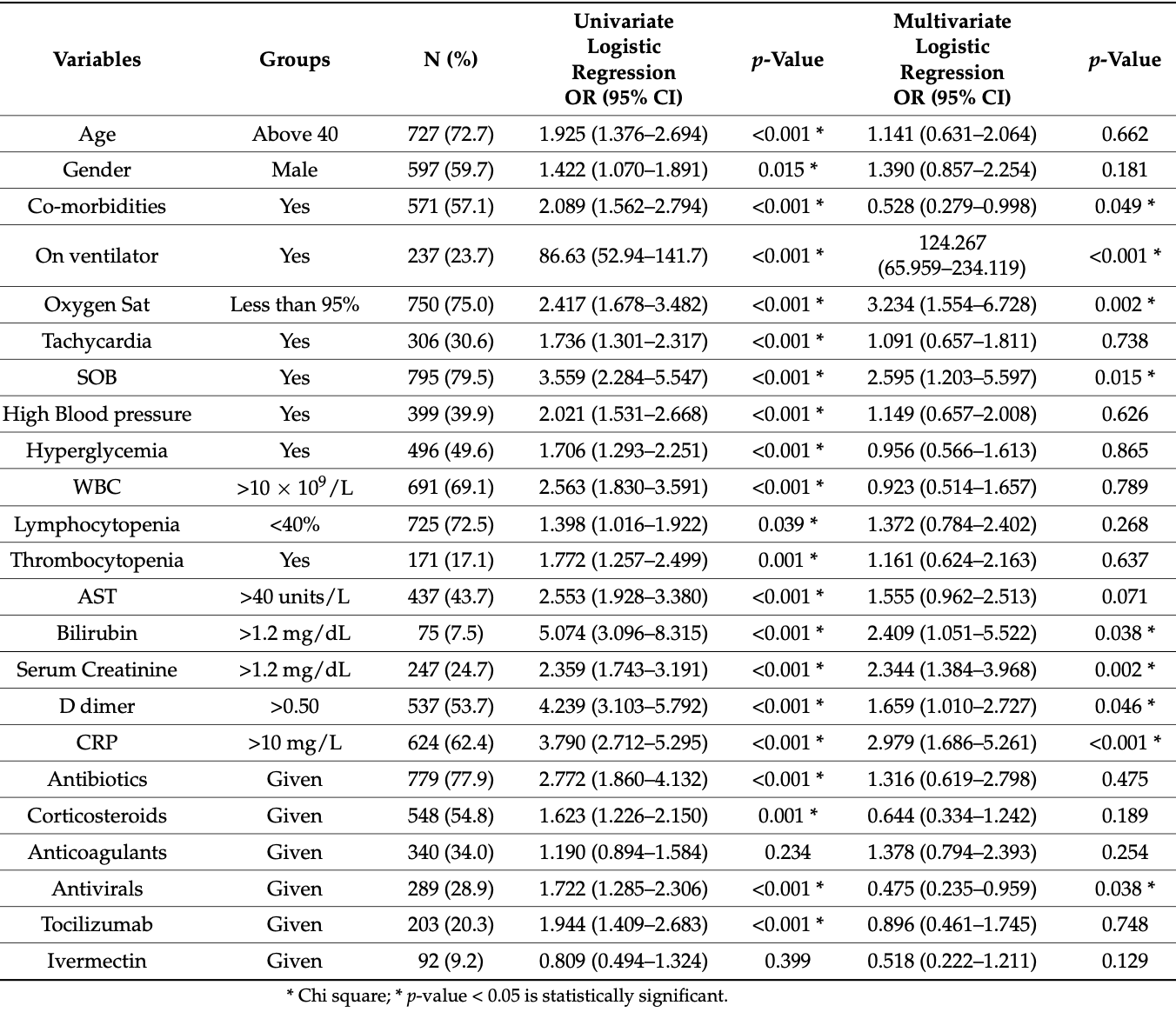
Background: Data on Pakistani COVID-19 patient mortality predictors is limited. It is essential to comprehend the relationship between disease characteristics, medications used, and mortality for better patient outcomes. Methods: The medical records of confirmed cases in the Lahore and Sargodha districts were examined using a two-stage cluster sampling from March 2021 to March 2022. Demographics, signs and symptoms, laboratory findings, and pharmacological medications as mortality indicators were noted and analyzed. Results: A total of 288 deaths occurred out of the 1000 cases. Death rates were higher for males and people over 40. Most of those who were mechanically ventilated perished (OR: 124.2). Dyspnea, fever, and cough were common symptoms, with a significant association amid SpO2 < 95% (OR: 3.2), RR > 20 breaths/min (OR: 2.5), and mortality. Patients with renal (OR: 2.3) or liver failure (OR: 1.5) were at risk. Raised C-reactive protein (OR: 2.9) and D-dimer levels were the indicators of mortality (OR: 1.6). The most prescribed drugs were antibiotics, (77.9%), corticosteroids (54.8%), anticoagulants (34%), tocilizumab (20.3%), and ivermectin (9.2%). Conclusions: Older males having breathing difficulties or signs of organ failure with raised C-reactive protein or D-dimer levels had high mortality. Antivirals, corticosteroids, tocilizumab, and ivermectin had better outcomes; antivirals were associated with lower mortality risk.
Author Contributions: Elements of this work including the conception of ideas, literature search, study designs, clinical data collections, statistical data analysis, data interpretation, manuscript drafting, and paper writing were done by M.Z.M., T.M.K. and A.H.K. Supervised and performed project administration, critical revisions of the paper, final editing, agreed to submit the manuscript to this journal, gave the final approval for the submitted version, and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: The authors declare no conflict of interest.
References
Akhtar, Akhtar, Rahman, Afridi, Khalid et al., An overview of the treatment options used for the management of COVID-19 in Pakistan: Retrospective observational study, JMIR Public Health Surveill,
doi:10.2196/28594Al-Kuraishy, Al-Gareeb, Bungau, Radu, Batiha, The potential molecular implications of adiponectin in the evolution of SARS-CoV-2: Inbuilt tendency, J. King Saud Univ.-Sci,
doi:10.1016/j.jksus.2022.102347Al-Saadi, Abdulnabi, Abdulnabi, Hematological changes associated with COVID-19 infection, J. Clin. Lab. Anal,
doi:10.1002/jcla.24064Alqahtani, Schattenberg, Liver injury in COVID-19: The current evidence, United Eur. Gastroenterol. J
Alvarez, Cabia, Trigo, Bandrés, Bestué, Prescription profile in patients with SARS-CoV-2 infection hospitalised in Aragon, Spain, Eur. J. Hosp. Pharm,
doi:10.1136/ejhpharm-2020-002476Beigel, Tomashek, Dodd, Mehta, Zingman et al., Remdesivir for the treatment of COVID-19, N. Engl. J. Med,
doi:10.1056/NEJMoa2007764Best, Kong, Kaplan-Lewis, Brawley, Baden et al., Treatment patterns in US patients hospitalized with COVID-19 and pulmonary involvement, J. Med. Virol,
doi:10.1002/jmv.27049Bhimraj, Morgan, Shumaker, Lavergne, Baden et al., Infectious Diseases Society of America Guidelines on the treatment and management of patients with coronavirus disease 2019 (COVID-19), Clin. Infect. Dis,
doi:10.1093/cid/ciaa478Boban, Novel coronavirus disease (COVID-19) update on epidemiology, pathogenicity, clinical course and treatments, Int. J. Clin. Pract,
doi:10.1111/ijcp.13868Bode, Garrett, Messler, Mcfarland, Crowe et al., Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States, J. Diabetes Sci. Technol,
doi:10.1177/1932296820924469Bogdanić, Močibob, Vidović, Soldo, Begovać, Azithromycin consumption during the COVID-19 pandemic in Croatia, PLoS ONE
Calderón-Parra, Cuervas-Mons, Moreno-Torres, Rubio-Rivas, Agudo-De Blas et al., Influence of chronic use of corticosteroids and calcineurin inhibitors on COVID-19 clinical outcomes: Analysis of a nationwide registry, Int. J. Infect. Dis
Capalbo, Aceti, Simmaco, Bonfini, Rocco et al., The exponential phase of the Covid-19 pandemic in central Italy: An integrated care pathway, Int. J. Environ. Res. Public Health,
doi:10.3390/ijerph17113792Chen, Li, Chen, Feng, Xiong, The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2, Cardiovasc. Res,
doi:10.1093/cvr/cvaa078Coronavirus, None
Cuker, Tseng, Nieuwlaat, Angchaisuksiri, Blair et al., American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: July 2021 update on postdischarge thromboprophylaxis, Blood Adv,
doi:10.1182/bloodadvances.2021005945Danilczyk, Penninger, Angiotensin-converting enzyme II in the heart and the kidney, Circ. Res
Deng, Liu, Liu, Fang, Shang et al., Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: A retrospective study, Chin. Med. J
Di Filippo, De Lorenzo, Sciorati, Capobianco, Lorè et al., Adiponectin to leptin ratio reflects inflammatory burden and survival in COVID-19, Diabetes Metab,
doi:10.1016/j.diabet.2021.101268Diaz, García, Muñoz, Perez, Gonzalez et al., Does timing matter on tocilizumab administration? Clinical, analytical and radiological outcomes in COVID-19, Eur. J. Hosp. Pharm,
doi:10.1136/ejhpharm-2020-002669Filion, Azoulay, Platt, Dahl, Dormuth et al., A multicenter observational study of incretin-based drugs and heart failure, N. Engl. J. Med,
doi:10.1056/NEJMoa1506115Gadi, Wu, Spihlman, Moulton, What's sex got to do with COVID-19? Gender-based differences in the host immune response to coronaviruses, Front. Immunol,
doi:10.3389/fimmu.2020.02147Gaertner, Massberg, Blood coagulation in immunothrombosis-At the frontline of intravascular immunity
Gao, Cai, Zhang, Zhou, Zhang et al., Association of hypertension and antihypertensive treatment with COVID-19 mortality: A retrospective observational study, Eur. Heart J
Goel, Goyal, Nagaraja, Kumar, Systemic corticosteroids for management of 'long-COVID': An evaluation after 3 months of treatment, Monaldi Arch. Chest Dis,
doi:10.4081/monaldi.2021.1981Goh, Choong, Cheong, Kalimuddin, Wen et al., Rapid progression to acute respiratory distress syndrome: Review of current understanding of critical illness from coronavirus disease 2019 (COVID-19) infection, Ann. Acad. Med. Singap,
doi:10.47102/annals-acadmedsg.202057Gottlieb, Vaca, Paredes, Mera, Webb et al., Early remdesivir to prevent progression to severe Covid-19 in outpatients, N. Engl. J. Med,
doi:10.1056/NEJMoa2116846Grasselli, Pesenti, Cecconi, Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response, JAMA,
doi:10.1001/jama.2020.4031Guo, Wei, Li, Li, Yang et al., Single-cell RNA analysis on ACE2 expression provides insights into SARS-CoV-2 potential entry into the bloodstream and heart injury, J. Cell. Physiol,
doi:10.1002/jcp.29802Harbuwono, Handayani, Wahyuningsih, Supraptowati, Kurniawan et al., Impact of diabetes mellitus on COVID-19 clinical symptoms and mortality: Jakarta's COVID-19 epidemiological registry, Prim. Care Diabetes,
doi:10.1016/j.pcd.2021.11.002Hashim, Alsuwaidi, Khan, Population risk factors for COVID-19 mortality in 93 countries, J. Epidemiol. Glob. Health,
doi:10.2991/jegh.k.200721.001Hu, Zhan, Chen, Ai, Xia, Chest CT findings related to mortality of patients with COVID-19: A retrospective case-series study, PLoS ONE,
doi:10.1371/journal.pone.0237302Hueda-Zavaleta, Copaja-Corzo, Bardales-Silva, Flores-Palacios, Barreto-Rocchetti et al., Factors associated with mortality due to COVID-19 in patients from a public hospital in Tacna, Peru. Rev. Peru, De Med. Exp. Y Salud Publica,
doi:10.17843/rpmesp.2021.382.7158Ionescu, Jaiyesimi, Petrescu, Lawler, Castillo et al., Association of anticoagulation dose and survival in hospitalized COVID-19 patients: A retrospective propensity score-weighted analysis, Eur. J. Haematol,
doi:10.1111/ejh.13533Jalil, Shanshool, Dilfy, Saleh, Suleiman, Hematological and serological parameters for detection of COVID-19, J. Microbiol. Biotechnol. Food Sci,
doi:10.55251/jmbfs.4229Jankauskas, Pevzner, Andrianova, Zorova, Popkov et al., The age-associated loss of ischemic preconditioning in the kidney is accompanied by mitochondrial dysfunction, increased protein acetylation and decreased autophagy, Sci. Rep,
doi:10.1038/srep44430Jin, Bai, He, Wu, Liu et al., Gender differences in patients with COVID-19: Focus on severity and mortality, Front. Public Health,
doi:10.3389/fpubh.2020.00152Kaftan, Hussain, Algenabi, Naser, Enaya, Predictive Value of C-reactive Protein, Lactate Dehydrogenase, Ferritin and D-dimer Levels in Diagnosing COVID-19 Patients: A Retrospective Study, Acta Inform. Med,
doi:10.5455/aim.2021.29.45-50Kaufman, Naidu, Ramachandran, Kaufman, Fayad et al., Review of radiographic findings in COVID-19, World J. Radiol,
doi:10.4329/wjr.v12.i8.142Kearns, Ahern, Patrie, Horton, Harris et al., Reduced adiponectin levels in patients with COVID-19 acute respiratory failure: A case-control study, Physiol. Rep,
doi:10.14814/phy2.14843Khaw, Richardson, Bhowmik, Agbetile, Rajakulasingam, Use of Corticosteroid in Persistent Post-COVID-19 Interstitial Lung Disease, Ann. Am. Thorac. Soc,
doi:10.1513/AnnalsATS.202105-623LEKonter, Parker, Baez, Li, Ranscht et al., Adiponectin attenuates lipopolysaccharide-induced acute lung injury through suppression of endothelial cell activation, J. Immunol,
doi:10.4049/jimmunol.1100426Kucharski, Russell, Diamond, Liu, Edmunds et al., Early dynamics of transmission and control of COVID-19: A mathematical modelling study, Lancet Infect. Dis
Kumar, Patel, Hererra, Jefferies, Sakhuja et al., Do high-dose corticosteroids improve outcomes in hospitalized COVID-19 patients?, J. Med. Virol,
doi:10.1002/jmv.27357Lai, Chen, Wang, Chen, Wang et al., Clinical efficacy and safety of remdesivir in patients with COVID-19: A systematic review and network meta-analysis of randomized controlled trials, J. Antimicrob. Chemother,
doi:10.1093/jac/dkab093Langford, So, Raybardhan, Leung, Soucy et al., Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis, Clin. Microbiol. Infect,
doi:10.1016/j.cmi.2020.12.018Mangkuliguna, Pramono, Efficacy and Safety of Azithromycin for the Treatment of COVID-19: A Systematic Review and Meta-analysis, Tuberc. Respir. Dis,
doi:10.4046/trd.2021.0075Martínez-Sanz, Muriel, Ron, Herrera, Pérez-Molina et al., Effects of tocilizumab on mortality in hospitalized patients with COVID-19: A multicentre cohort study, Clin. Microbiol. Infect,
doi:10.1016/j.cmi.2020.09.021Musoke, Lo, Albano, Peterson, Bhargav et al., None
Nishiga, Wang, Han, Lewis, Wu, COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives, Nat. Rev. Cardiol,
doi:10.1038/s41569-020-0413-9Onder, Rezza, Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA,
doi:10.1001/jama.2020.4683Opal, Girard, Ely, The immunopathogenesis of sepsis in elderly patients, Clin. Infect. Dis,
doi:10.1086/432007Ospina-Tascón, Calderón-Tapia, García, Zarama, Gómez-Álvarez et al., Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with severe COVID-19: A randomized clinical trial, JAMA,
doi:10.1001/jama.2021.20714Panel, COVID-19) Treatment Guidelines
Pennington, Kompaniyets, Summers, Danielson, Goodman et al., Risk of clinical severity by age and race/ethnicity among adults hospitalized for COVID-19-United States
Qin, Dong, Zhang, Hu, Chen et al., Low molecular weight heparin and 28-day mortality among patients with coronavirus disease 2019: A cohort study in the early epidemic era, Thromb. Res,
doi:10.1016/j.thromres.2020.11.020Querequincia, Faller, A systematic review on the clinical studies of Remdesivir for COVID-19 in selected Asian countries, J. Appl. Pharm. Sci
Rajter, Sherman, Fatteh, Vogel, Sacks et al., Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: The ivermectin in COVID nineteen study, Chest,
doi:10.1016/j.chest.2020.10.009Rashedi, Mahdavi Poor, Asgharzadeh, Pourostadi, Samadi Kafil et al., Risk Factors for COVID-19, Infez. Med
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA,
doi:10.1001/jama.2020.6775Robinson, Mchugh, Mandalapu, Clay, Lee et al., Influenza A virus exacerbates Staphylococcus aureus pneumonia in mice by attenuating antimicrobial peptide production, J. Infect. Dis,
doi:10.1093/infdis/jit527Rozenfeld, Beam, Maier, Haggerson, Boudreau et al., A model of disparities: Risk factors associated with COVID-19 infection, Int. J. Equity Health,
doi:10.1186/s12939-020-01242-zRubino, Amiel, Zimmet, Alberti, Bornstein et al., New-onset diabetes in COVID-19, N. Engl. J. Med,
doi:10.1056/NEJMc2018688Schulman, Sholzberg, Spyropoulos, Zarychanski, Resnick et al., ISTH guidelines for antithrombotic treatment in COVID-19, J. Thromb. Haemost
Shah, Majmudar, Stein, Gupta, Suppes et al., Novel use of home pulse oximetry monitoring in COVID-19 patients discharged from the emergency department identifies need for hospitalization, Acad. Emerg. Med,
doi:10.1111/acem.14053Shimizu, Hirata, Kabata, Tokuhira, Koide et al., Ivermectin administration is associated with lower gastrointestinal complications and greater ventilator-free days in ventilated patients with COVID-19: A propensity score analysis, J. Infect. Chemother,
doi:10.1016/j.jiac.2021.12.024Smilowitz, Kunichoff, Garshick, Shah, Pillinger et al., C-reactive protein and clinical outcomes in patients with COVID-19, Eur. Heart J,
doi:10.1093/eurheartj/ehaa1103Suardi, Pallotto, Esperti, Tazzioli, Baragli et al., Risk factors for non-invasive/invasive ventilatory support in patients with COVID-19 pneumonia: A retrospective study within a multidisciplinary approach, Int. J. Infect. Dis,
doi:10.1016/j.ijid.2020.09.012Sun, Kou, Wang, Lu, Zhao et al., An analytical study of drug utilization, disease progression, and adverse events among 165 COVID-19 patients, Ann. Transl. Med,
doi:10.21037/atm-20-4960Tamez-Pérez, Quintanilla-Flores, Rodríguez-Gutiérrez, González-González, Tamez-Peña, Steroid hyperglycemia: Prevalence, early detection and therapeutic recommendations: A narrative review, World J. Diabetes
Tan, Song, Deane, Plummer, Global impact of coronavirus disease 2019 infection requiring admission to the ICU: A systematic review and meta-analysis, Chest,
doi:10.1016/j.chest.2020.10.014Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J. Thromb. Haemost,
doi:10.1111/jth.14768Toroghi, Abbasian, Nourian, Davoudi-Monfared, Khalili et al., Comparing efficacy and safety of different doses of dexamethasone in the treatment of COVID-19: A three-arm randomized clinical trial, Pharmacol. Rep,
doi:10.1007/s43440-021-00341-0Vallianou, Tsilingiris, Christodoulatos, Karampela, Dalamaga, Anti-viral treatment for SARS-CoV-2 infection: A race against time amidst the ongoing pandemic, Metab. Open,
doi:10.1016/j.metop.2021.100096Wang, Luo, Zhang, Yu, Cheng et al., The involvement of chronic kidney disease and acute kidney injury in disease severity and mortality in patients with COVID-19: A meta-analysis, Kidney Blood Press. Res,
doi:10.1159/000512211Wang, Yao, Liu, Cao, Wang et al., Risk factors of coronavirus disease 2019-related mortality and optimal treatment regimens: A retrospective study, Med. Sci. Monit. Int. Med. J. Exp. Clin. Res,
doi:10.12659/MSM.926751Watanabe, Kwon, Nan, Abeles, Jia et al., Medication use patterns in hospitalized patients with COVID-19 in California during the pandemic, JAMA Netw. Open,
doi:10.1001/jamanetworkopen.2021.10775Wu, Huang, Zhu, Wang, Lv et al., Elevation of blood glucose level predicts worse outcomes in hospitalized patients with COVID-19: A retrospective cohort study, BMJ Open Diabetes Res. Care,
doi:10.1136/bmjdrc-2020-001476Xu, Zhong, Deng, Peng, Dan et al., High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, Int. J. Oral Sci,
doi:10.1038/s41368-020-0074-xYang, Lin, Ji, Guo, Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes, Acta Diabetol,
doi:10.1007/s00592-009-0109-4Yu, Koh, Choi, Ryoo, Huh et al., Clinical efficacy and safety of interleukin-6 receptor antagonists (tocilizumab and sarilumab) in patients with COVID-19: A systematic review and meta-analysis, Emerg. Microbes Infect,
doi:10.1080/22221751.2022.2059405Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.3390/healthcare11081192",
"ISSN": [
"2227-9032"
],
"URL": "http://dx.doi.org/10.3390/healthcare11081192",
"abstract": "<jats:p>Background: Data on Pakistani COVID-19 patient mortality predictors is limited. It is essential to comprehend the relationship between disease characteristics, medications used, and mortality for better patient outcomes. Methods: The medical records of confirmed cases in the Lahore and Sargodha districts were examined using a two-stage cluster sampling from March 2021 to March 2022. Demographics, signs and symptoms, laboratory findings, and pharmacological medications as mortality indicators were noted and analyzed. Results: A total of 288 deaths occurred out of the 1000 cases. Death rates were higher for males and people over 40. Most of those who were mechanically ventilated perished (OR: 124.2). Dyspnea, fever, and cough were common symptoms, with a significant association amid SpO2 < 95% (OR: 3.2), RR > 20 breaths/min (OR: 2.5), and mortality. Patients with renal (OR: 2.3) or liver failure (OR: 1.5) were at risk. Raised C-reactive protein (OR: 2.9) and D-dimer levels were the indicators of mortality (OR: 1.6). The most prescribed drugs were antibiotics, (77.9%), corticosteroids (54.8%), anticoagulants (34%), tocilizumab (20.3%), and ivermectin (9.2%). Conclusions: Older males having breathing difficulties or signs of organ failure with raised C-reactive protein or D-dimer levels had high mortality. Antivirals, corticosteroids, tocilizumab, and ivermectin had better outcomes; antivirals were associated with lower mortality risk.</jats:p>",
"alternative-id": [
"healthcare11081192"
],
"author": [
{
"affiliation": [
{
"name": "Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Gelugor 11800, Penang, Malaysia"
},
{
"name": "Institute of Pharmaceutical Sciences, University of Veterinary and Animal Sciences, Syed Abdul Qadir Jillani (Out Fall) Road, Lahore 54000, Pakistan"
}
],
"family": "Munir",
"given": "Muhammad Zeeshan",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-4802-6181",
"affiliation": [
{
"name": "Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Gelugor 11800, Penang, Malaysia"
}
],
"authenticated-orcid": false,
"family": "Khan",
"given": "Amer Hayat",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Institute of Pharmaceutical Sciences, University of Veterinary and Animal Sciences, Syed Abdul Qadir Jillani (Out Fall) Road, Lahore 54000, Pakistan"
},
{
"name": "School of Pharmacy, Monash University Malaysia Sdn Bhd, Jalan Lagoon Selatan, Banday Sunway, Subang Jaya 45700, Selangor, Malaysia"
}
],
"family": "Khan",
"given": "Tahir Mehmood",
"sequence": "additional"
}
],
"container-title": "Healthcare",
"container-title-short": "Healthcare",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
21
]
],
"date-time": "2023-04-21T06:05:31Z",
"timestamp": 1682057131000
},
"deposited": {
"date-parts": [
[
2023,
12,
11
]
],
"date-time": "2023-12-11T05:14:45Z",
"timestamp": 1702271685000
},
"indexed": {
"date-parts": [
[
2023,
12,
11
]
],
"date-time": "2023-12-11T05:46:55Z",
"timestamp": 1702273615407
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2023,
4,
21
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2023,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
4,
21
]
],
"date-time": "2023-04-21T00:00:00Z",
"timestamp": 1682035200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9032/11/8/1192/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1192",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
4,
21
]
]
},
"published-online": {
"date-parts": [
[
2023,
4,
21
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.chest.2020.10.014",
"article-title": "Global impact of coronavirus disease 2019 infection requiring admission to the ICU: A systematic review and meta-analysis",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "524",
"journal-title": "Chest",
"key": "ref_1",
"volume": "159",
"year": "2021"
},
{
"DOI": "10.47102/annals-acadmedsg.202057",
"article-title": "Rapid progression to acute respiratory distress syndrome: Review of current understanding of critical illness from coronavirus disease 2019 (COVID-19) infection",
"author": "Goh",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "Ann. Acad. Med. Singap.",
"key": "ref_2",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.4031",
"article-title": "Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response",
"author": "Grasselli",
"doi-asserted-by": "crossref",
"first-page": "1545",
"journal-title": "JAMA",
"key": "ref_3",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1186/s12939-020-01242-z",
"article-title": "A model of disparities: Risk factors associated with COVID-19 infection",
"author": "Rozenfeld",
"doi-asserted-by": "crossref",
"first-page": "126",
"journal-title": "Int. J. Equity Health",
"key": "ref_4",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"journal-title": "Lancet",
"key": "ref_5",
"volume": "395",
"year": "2020"
},
{
"key": "ref_6",
"unstructured": "Pennington, A.F., Kompaniyets, L., Summers, A.D., Danielson, M.L., Goodman, A.B., Chevinsky, J.R., Preston, L.E., Schieber, L.Z., Namulanda, G., and Courtney, J. (2021). Open Forum Infectious Diseases, Oxford University Press US."
},
{
"article-title": "Risk Factors for COVID-19",
"author": "Rashedi",
"first-page": "469",
"journal-title": "Infez. Med.",
"key": "ref_7",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.2991/jegh.k.200721.001",
"article-title": "Population risk factors for COVID-19 mortality in 93 countries",
"author": "Hashim",
"doi-asserted-by": "crossref",
"first-page": "204",
"journal-title": "J. Epidemiol. Glob. Health",
"key": "ref_8",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1152/ajpendo.00124.2020",
"article-title": "COVID-19 pandemic, coronaviruses, and diabetes mellitus",
"author": "Muniyappa",
"doi-asserted-by": "crossref",
"first-page": "E736",
"journal-title": "Am. J. Physiol.-Endocrinol. Metab.",
"key": "ref_9",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa433",
"article-title": "Association of hypertension and antihypertensive treatment with COVID-19 mortality: A retrospective observational study",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "2058",
"journal-title": "Eur. Heart J.",
"key": "ref_10",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0413-9",
"article-title": "COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives",
"author": "Nishiga",
"doi-asserted-by": "crossref",
"first-page": "543",
"journal-title": "Nat. Rev. Cardiol.",
"key": "ref_11",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.5455/aim.2021.29.45-50",
"article-title": "Predictive Value of C–reactive Protein, Lactate Dehydrogenase, Ferritin and D-dimer Levels in Diagnosing COVID-19 Patients: A Retrospective Study",
"author": "Kaftan",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Acta Inform. Med.",
"key": "ref_12",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.jksus.2022.102347",
"article-title": "The potential molecular implications of adiponectin in the evolution of SARS-CoV-2: Inbuilt tendency",
"author": "Bungau",
"doi-asserted-by": "crossref",
"first-page": "102347",
"journal-title": "J. King Saud Univ.-Sci.",
"key": "ref_13",
"volume": "34",
"year": "2022"
},
{
"DOI": "10.4049/jimmunol.1100426",
"article-title": "Adiponectin attenuates lipopolysaccharide-induced acute lung injury through suppression of endothelial cell activation",
"author": "Konter",
"doi-asserted-by": "crossref",
"first-page": "854",
"journal-title": "J. Immunol.",
"key": "ref_14",
"volume": "188",
"year": "2012"
},
{
"DOI": "10.14814/phy2.14843",
"article-title": "Reduced adiponectin levels in patients with COVID-19 acute respiratory failure: A case-control study",
"author": "Kearns",
"doi-asserted-by": "crossref",
"first-page": "e14843",
"journal-title": "Physiol. Rep.",
"key": "ref_15",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.diabet.2021.101268",
"article-title": "Adiponectin to leptin ratio reflects inflammatory burden and survival in COVID-19",
"author": "Sciorati",
"doi-asserted-by": "crossref",
"first-page": "101268",
"journal-title": "Diabetes Metab.",
"key": "ref_16",
"volume": "47",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2020.09.012",
"article-title": "Risk factors for non-invasive/invasive ventilatory support in patients with COVID-19 pneumonia: A retrospective study within a multidisciplinary approach",
"author": "Suardi",
"doi-asserted-by": "crossref",
"first-page": "258",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_17",
"volume": "100",
"year": "2020"
},
{
"DOI": "10.1097/CM9.0000000000000824",
"article-title": "Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: A retrospective study",
"author": "Deng",
"doi-asserted-by": "crossref",
"first-page": "1261",
"journal-title": "Chin. Med. J.",
"key": "ref_18",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.4329/wjr.v12.i8.142",
"article-title": "Review of radiographic findings in COVID-19",
"author": "Kaufman",
"doi-asserted-by": "crossref",
"first-page": "142",
"journal-title": "World J. Radiol.",
"key": "ref_19",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0237302",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Hu, Y., Zhan, C., Chen, C., Ai, T., and Xia, L. (2020). Chest CT findings related to mortality of patients with COVID-19: A retrospective case-series study. PLoS ONE, 15."
},
{
"DOI": "10.1016/S1473-3099(20)30144-4",
"article-title": "Early dynamics of transmission and control of COVID-19: A mathematical modelling study",
"author": "Kucharski",
"doi-asserted-by": "crossref",
"first-page": "553",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_21",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1080/23744235.2020.1748705",
"article-title": "Duration of SARS-CoV-2 viral shedding during COVID-19 infection",
"author": "Qian",
"doi-asserted-by": "crossref",
"first-page": "511",
"journal-title": "Infect. Dis.",
"key": "ref_22",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1016/j.nmni.2020.100681",
"article-title": "COVID-19 outbreak: Current scenario of Pakistan",
"author": "Waris",
"doi-asserted-by": "crossref",
"first-page": "100681",
"journal-title": "New Microbes New Infect.",
"key": "ref_23",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1111/ijcp.13868",
"article-title": "Novel coronavirus disease (COVID-19) update on epidemiology, pathogenicity, clinical course and treatments",
"author": "Boban",
"doi-asserted-by": "crossref",
"first-page": "e13868",
"journal-title": "Int. J. Clin. Pract.",
"key": "ref_24",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2007764",
"article-title": "Remdesivir for the treatment of COVID-19",
"author": "Beigel",
"doi-asserted-by": "crossref",
"first-page": "1813",
"journal-title": "N. Engl. J. Med.",
"key": "ref_25",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1016/j.metop.2021.100096",
"article-title": "Anti-viral treatment for SARS-CoV-2 infection: A race against time amidst the ongoing pandemic",
"author": "Vallianou",
"doi-asserted-by": "crossref",
"first-page": "100096",
"journal-title": "Metab. Open",
"key": "ref_26",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1007/s40265-020-01367-z",
"article-title": "Pharmaco-immunomodulatory therapy in COVID-19",
"author": "Rizk",
"doi-asserted-by": "crossref",
"first-page": "1267",
"journal-title": "Drugs",
"key": "ref_27",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1001/jama.2021.20714",
"article-title": "Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with severe COVID-19: A randomized clinical trial",
"author": "Zarama",
"doi-asserted-by": "crossref",
"first-page": "2161",
"journal-title": "JAMA",
"key": "ref_28",
"volume": "326",
"year": "2021"
},
{
"DOI": "10.1016/j.transci.2020.102790",
"article-title": "Treatment for emerging viruses: Convalescent plasma and COVID-19",
"author": "Brown",
"doi-asserted-by": "crossref",
"first-page": "102790",
"journal-title": "Transfus. Apher. Sci.",
"key": "ref_29",
"volume": "59",
"year": "2020"
},
{
"DOI": "10.1111/ejh.13533",
"article-title": "Association of anticoagulation dose and survival in hospitalized COVID-19 patients: A retrospective propensity score-weighted analysis",
"author": "Ionescu",
"doi-asserted-by": "crossref",
"first-page": "165",
"journal-title": "Eur. J. Haematol.",
"key": "ref_30",
"volume": "106",
"year": "2021"
},
{
"article-title": "Risk factors of coronavirus disease 2019-related mortality and optimal treatment regimens: A retrospective study",
"author": "Wang",
"first-page": "e926751-1",
"journal-title": "Med. Sci. Monit. Int. Med. J. Exp. Clin. Res.",
"key": "ref_31",
"volume": "27",
"year": "2021"
},
{
"article-title": "Factors associated with mortality due to COVID-19 in patients from a public hospital in Tacna, Peru",
"first-page": "214",
"journal-title": "Rev. Peru. De Med. Exp. Y Salud Publica",
"key": "ref_32",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"journal-title": "JAMA",
"key": "ref_33",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1086/432007",
"article-title": "The immunopathogenesis of sepsis in elderly patients",
"author": "Opal",
"doi-asserted-by": "crossref",
"first-page": "S504",
"journal-title": "Clin. Infect. Dis.",
"key": "ref_34",
"volume": "41",
"year": "2005"
},
{
"DOI": "10.1038/srep44430",
"article-title": "The age-associated loss of ischemic preconditioning in the kidney is accompanied by mitochondrial dysfunction, increased protein acetylation and decreased autophagy",
"author": "Jankauskas",
"doi-asserted-by": "crossref",
"first-page": "44430",
"journal-title": "Sci. Rep.",
"key": "ref_35",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.2196/28594",
"article-title": "An overview of the treatment options used for the management of COVID-19 in Pakistan: Retrospective observational study",
"author": "Akhtar",
"doi-asserted-by": "crossref",
"first-page": "e28594",
"journal-title": "JMIR Public Health Surveill.",
"key": "ref_36",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.02147",
"article-title": "What’s sex got to do with COVID-19? Gender-based differences in the host immune response to coronaviruses",
"author": "Gadi",
"doi-asserted-by": "crossref",
"first-page": "2147",
"journal-title": "Front. Immunol.",
"key": "ref_37",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.00152",
"article-title": "Gender differences in patients with COVID-19: Focus on severity and mortality",
"author": "Jin",
"doi-asserted-by": "crossref",
"first-page": "152",
"journal-title": "Front. Public Health",
"key": "ref_38",
"volume": "8",
"year": "2020"
},
{
"key": "ref_39",
"unstructured": "(2022, September 15). COVID-19 Dashboard. Available online: https://coronaboard.kr/."
},
{
"key": "ref_40",
"unstructured": "(2022, April 20). Nuovo Coronavirus, Available online: https://www.salute.gov.it/portale/home.html."
},
{
"article-title": "Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy",
"author": "Onder",
"first-page": "1775",
"journal-title": "JAMA",
"key": "ref_41",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3390/ijerph17113792",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "Capalbo, C., Aceti, A., Simmaco, M., Bonfini, R., Rocco, M., Ricci, A., Napoli, C., Rocco, M., Alfonsi, V., and Teggi, A. (2020). The exponential phase of the Covid-19 pandemic in central Italy: An integrated care pathway. Int. J. Environ. Res. Public Health, 17."
},
{
"DOI": "10.1016/j.pcd.2021.11.002",
"article-title": "Impact of diabetes mellitus on COVID-19 clinical symptoms and mortality: Jakarta’s COVID-19 epidemiological registry",
"author": "Harbuwono",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Prim. Care Diabetes",
"key": "ref_43",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1056/NEJMc2018688",
"article-title": "New-onset diabetes in COVID-19",
"author": "Rubino",
"doi-asserted-by": "crossref",
"first-page": "789",
"journal-title": "N. Engl. J. Med.",
"key": "ref_44",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1007/s00592-009-0109-4",
"article-title": "Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "193",
"journal-title": "Acta Diabetol.",
"key": "ref_45",
"volume": "47",
"year": "2010"
},
{
"DOI": "10.1002/jcp.29802",
"article-title": "Single-cell RNA analysis on ACE2 expression provides insights into SARS-CoV-2 potential entry into the bloodstream and heart injury",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "9884",
"journal-title": "J. Cell. Physiol.",
"key": "ref_46",
"volume": "235",
"year": "2020"
},
{
"DOI": "10.1093/cvr/cvaa078",
"article-title": "The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1097",
"journal-title": "Cardiovasc. Res.",
"key": "ref_47",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1161/CIRCRESAHA.121.318054",
"article-title": "Hypertension, a moving target in COVID-19: Current views and perspectives",
"author": "Savoia",
"doi-asserted-by": "crossref",
"first-page": "1062",
"journal-title": "Circ. Res.",
"key": "ref_48",
"volume": "128",
"year": "2021"
},
{
"DOI": "10.1111/acem.14053",
"article-title": "Novel use of home pulse oximetry monitoring in COVID-19 patients discharged from the emergency department identifies need for hospitalization",
"author": "Shah",
"doi-asserted-by": "crossref",
"first-page": "681",
"journal-title": "Acad. Emerg. Med.",
"key": "ref_49",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.55251/jmbfs.4229",
"article-title": "Hematological and serological parameters for detection of COVID-19",
"author": "Jalil",
"doi-asserted-by": "crossref",
"first-page": "e4229",
"journal-title": "J. Microbiol. Biotechnol. Food Sci.",
"key": "ref_50",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1002/jcla.24064",
"article-title": "Hematological changes associated with COVID-19 infection",
"author": "Abdulnabi",
"doi-asserted-by": "crossref",
"first-page": "e24064",
"journal-title": "J. Clin. Lab. Anal.",
"key": "ref_51",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1177/1932296820924469",
"article-title": "Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States",
"author": "Bode",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "J. Diabetes Sci. Technol.",
"key": "ref_52",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1136/bmjdrc-2020-001476",
"article-title": "Elevation of blood glucose level predicts worse outcomes in hospitalized patients with COVID-19: A retrospective cohort study",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "e001476",
"journal-title": "BMJ Open Diabetes Res. Care",
"key": "ref_53",
"volume": "8",
"year": "2020"
},
{
"key": "ref_54",
"unstructured": "Gaertner, F., and Massberg, S. (2016). Seminars in Immunology, Elsevier."
},
{
"DOI": "10.1111/jth.14768",
"article-title": "Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "844",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_55",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1038/s41368-020-0074-x",
"article-title": "High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Int. J. Oral Sci.",
"key": "ref_56",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa1103",
"article-title": "C-reactive protein and clinical outcomes in patients with COVID-19",
"author": "Smilowitz",
"doi-asserted-by": "crossref",
"first-page": "2270",
"journal-title": "Eur. Heart J.",
"key": "ref_57",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.jhep.2020.04.006",
"article-title": "COVID-19: Abnormal liver function tests",
"author": "Cai",
"doi-asserted-by": "crossref",
"first-page": "566",
"journal-title": "J. Hepatol.",
"key": "ref_58",
"volume": "73",
"year": "2020"
},
{
"DOI": "10.1177/2050640620924157",
"article-title": "Liver injury in COVID-19: The current evidence",
"author": "Alqahtani",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "United Eur. Gastroenterol. J.",
"key": "ref_59",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1161/01.RES.0000205761.22353.5f",
"article-title": "Angiotensin-converting enzyme II in the heart and the kidney",
"author": "Danilczyk",
"doi-asserted-by": "crossref",
"first-page": "463",
"journal-title": "Circ. Res.",
"key": "ref_60",
"volume": "98",
"year": "2006"
},
{
"DOI": "10.1159/000512211",
"article-title": "The involvement of chronic kidney disease and acute kidney injury in disease severity and mortality in patients with COVID-19: A meta-analysis",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "17",
"journal-title": "Kidney Blood Press. Res.",
"key": "ref_61",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.21037/atm-20-4960",
"article-title": "An analytical study of drug utilization, disease progression, and adverse events among 165 COVID-19 patients",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "306",
"journal-title": "Ann. Transl. Med.",
"key": "ref_62",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.10775",
"article-title": "Medication use patterns in hospitalized patients with COVID-19 in California during the pandemic",
"author": "Watanabe",
"doi-asserted-by": "crossref",
"first-page": "e2110775",
"journal-title": "JAMA Netw. Open",
"key": "ref_63",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1136/ejhpharm-2020-002476",
"article-title": "Prescription profile in patients with SARS-CoV-2 infection hospitalised in Aragon, Spain",
"author": "Alvarez",
"doi-asserted-by": "crossref",
"first-page": "287",
"journal-title": "Eur. J. Hosp. Pharm.",
"key": "ref_64",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1002/jmv.27049",
"article-title": "Treatment patterns in US patients hospitalized with COVID-19 and pulmonary involvement",
"author": "Best",
"doi-asserted-by": "crossref",
"first-page": "5367",
"journal-title": "J. Med. Virol.",
"key": "ref_65",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.4046/trd.2021.0075",
"article-title": "Efficacy and Safety of Azithromycin for the Treatment of COVID-19: A Systematic Review and Meta-analysis",
"author": "Mangkuliguna",
"doi-asserted-by": "crossref",
"first-page": "299",
"journal-title": "Tuberc. Respir. Dis.",
"key": "ref_66",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2020.12.018",
"article-title": "Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis",
"author": "Langford",
"doi-asserted-by": "crossref",
"first-page": "520",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_67",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0263437",
"doi-asserted-by": "crossref",
"key": "ref_68",
"unstructured": "Bogdanić, N., Močibob, L., Vidović, T., Soldo, A., and Begovać, J. (2022). Azithromycin consumption during the COVID-19 pandemic in Croatia, 2020. PLoS ONE, 17."
},
{
"DOI": "10.1513/AnnalsATS.202105-623LE",
"article-title": "Use of Corticosteroid in Persistent Post–COVID-19 Interstitial Lung Disease",
"author": "Khaw",
"doi-asserted-by": "crossref",
"first-page": "1599",
"journal-title": "Ann. Am. Thorac. Soc.",
"key": "ref_69",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.ijid.2021.12.327",
"article-title": "Influence of chronic use of corticosteroids and calcineurin inhibitors on COVID-19 clinical outcomes: Analysis of a nationwide registry",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Int. J. Infect. Dis.",
"key": "ref_70",
"volume": "116",
"year": "2022"
},
{
"DOI": "10.1002/jmv.27357",
"article-title": "Do high-dose corticosteroids improve outcomes in hospitalized COVID-19 patients?",
"author": "Kumar",
"doi-asserted-by": "crossref",
"first-page": "372",
"journal-title": "J. Med. Virol.",
"key": "ref_71",
"volume": "94",
"year": "2022"
},
{
"article-title": "Systemic corticosteroids for management of ‘long-COVID’: An evaluation after 3 months of treatment",
"author": "Goel",
"first-page": "1981",
"journal-title": "Monaldi Arch. Chest Dis.",
"key": "ref_72",
"volume": "92",
"year": "2022"
},
{
"DOI": "10.1007/s43440-021-00341-0",
"article-title": "Comparing efficacy and safety of different doses of dexamethasone in the treatment of COVID-19: A three-arm randomized clinical trial",
"author": "Toroghi",
"doi-asserted-by": "crossref",
"first-page": "229",
"journal-title": "Pharmacol. Rep.",
"key": "ref_73",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.4239/wjd.v6.i8.1073",
"article-title": "Steroid hyperglycemia: Prevalence, early detection and therapeutic recommendations: A narrative review",
"doi-asserted-by": "crossref",
"first-page": "1073",
"journal-title": "World J. Diabetes",
"key": "ref_74",
"volume": "6",
"year": "2015"
},
{
"key": "ref_75",
"unstructured": "Panel, C.-T.G. (2020). Coronavirus Disease 2019 (COVID-19) Treatment Guidelines, National Institutes of Health."
},
{
"DOI": "10.1093/cid/ciaa478",
"doi-asserted-by": "crossref",
"key": "ref_76",
"unstructured": "Bhimraj, A., Morgan, R.L., Shumaker, A.H., Lavergne, V., Baden, L., Cheng, V.C.-C., Edwards, K.M., Gandhi, R., Muller, W.J., and O’Horo, J.C. (2020). Infectious Diseases Society of America Guidelines on the treatment and management of patients with coronavirus disease 2019 (COVID-19). Clin. Infect. Dis., ciaa478."
},
{
"DOI": "10.1016/j.thromres.2020.08.035",
"article-title": "Anticoagulation and bleeding risk in patients with COVID-19",
"author": "Musoke",
"doi-asserted-by": "crossref",
"first-page": "227",
"journal-title": "Thromb. Res.",
"key": "ref_77",
"volume": "196",
"year": "2020"
},
{
"DOI": "10.1016/j.thromres.2020.11.020",
"article-title": "Low molecular weight heparin and 28-day mortality among patients with coronavirus disease 2019: A cohort study in the early epidemic era",
"author": "Qin",
"doi-asserted-by": "crossref",
"first-page": "19",
"journal-title": "Thromb. Res.",
"key": "ref_78",
"volume": "198",
"year": "2021"
},
{
"DOI": "10.1182/blood.2020006000",
"article-title": "COVID-19 and its implications for thrombosis and anticoagulation",
"author": "Connors",
"doi-asserted-by": "crossref",
"first-page": "2033",
"journal-title": "Blood",
"key": "ref_79",
"volume": "135",
"year": "2020"
},
{
"DOI": "10.1182/bloodadvances.2021005945",
"article-title": "American Society of Hematology living guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID-19: July 2021 update on postdischarge thromboprophylaxis",
"author": "Cuker",
"doi-asserted-by": "crossref",
"first-page": "664",
"journal-title": "Blood Adv.",
"key": "ref_80",
"volume": "6",
"year": "2022"
},
{
"article-title": "Surviving COVID-19 with heparin?",
"first-page": "845",
"journal-title": "Mass. Med. Soc.",
"key": "ref_81",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(21)01291-5",
"article-title": "Anticoagulation in COVID-19: Reaction to the ACTION trial",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "2226",
"journal-title": "Lancet",
"key": "ref_82",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1111/jth.15808",
"article-title": "ISTH guidelines for antithrombotic treatment in COVID-19",
"author": "Schulman",
"doi-asserted-by": "crossref",
"first-page": "2214",
"journal-title": "J. Thromb. Haemost.",
"key": "ref_83",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1093/jac/dkab093",
"article-title": "Clinical efficacy and safety of remdesivir in patients with COVID-19: A systematic review and network meta-analysis of randomized controlled trials",
"author": "Lai",
"doi-asserted-by": "crossref",
"first-page": "1962",
"journal-title": "J. Antimicrob. Chemother.",
"key": "ref_84",
"volume": "76",
"year": "2021"
},
{
"article-title": "A systematic review on the clinical studies of Remdesivir for COVID-19 in selected Asian countries",
"author": "Querequincia",
"first-page": "10",
"journal-title": "J. Appl. Pharm. Sci.",
"key": "ref_85",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2116846",
"article-title": "Early remdesivir to prevent progression to severe Covid-19 in outpatients",
"author": "Gottlieb",
"doi-asserted-by": "crossref",
"first-page": "305",
"journal-title": "N. Engl. J. Med.",
"key": "ref_86",
"volume": "386",
"year": "2022"
},
{
"key": "ref_87",
"unstructured": "Infectious Diseases Society of America (2021). IDSA Guidelines on the Treatment and Management of Patients with COVID-19, Infectious Diseases Society of America."
},
{
"DOI": "10.1016/j.cmi.2020.09.021",
"article-title": "Effects of tocilizumab on mortality in hospitalized patients with COVID-19: A multicentre cohort study",
"author": "Muriel",
"doi-asserted-by": "crossref",
"first-page": "238",
"journal-title": "Clin. Microbiol. Infect.",
"key": "ref_88",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1093/infdis/jit527",
"article-title": "Influenza A virus exacerbates Staphylococcus aureus pneumonia in mice by attenuating antimicrobial peptide production",
"author": "Robinson",
"doi-asserted-by": "crossref",
"first-page": "865",
"journal-title": "J. Infect. Dis.",
"key": "ref_89",
"volume": "209",
"year": "2014"
},
{
"DOI": "10.1136/ejhpharm-2020-002669",
"article-title": "Does timing matter on tocilizumab administration? Clinical, analytical and radiological outcomes in COVID-19",
"author": "Diaz",
"doi-asserted-by": "crossref",
"first-page": "340",
"journal-title": "Eur. J. Hosp. Pharm.",
"key": "ref_90",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1080/22221751.2022.2059405",
"article-title": "Clinical efficacy and safety of interleukin-6 receptor antagonists (tocilizumab and sarilumab) in patients with COVID-19: A systematic review and meta-analysis",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "1154",
"journal-title": "Emerg. Microbes Infect.",
"key": "ref_91",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.chest.2020.10.009",
"article-title": "Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: The ivermectin in COVID nineteen study",
"author": "Rajter",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Chest",
"key": "ref_92",
"volume": "159",
"year": "2021"
},
{
"DOI": "10.1016/j.jiac.2021.12.024",
"article-title": "Ivermectin administration is associated with lower gastrointestinal complications and greater ventilator-free days in ventilated patients with COVID-19: A propensity score analysis",
"author": "Shimizu",
"doi-asserted-by": "crossref",
"first-page": "548",
"journal-title": "J. Infect. Chemother.",
"key": "ref_93",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa1506115",
"article-title": "A multicenter observational study of incretin-based drugs and heart failure",
"author": "Filion",
"doi-asserted-by": "crossref",
"first-page": "1145",
"journal-title": "N. Engl. J. Med.",
"key": "ref_94",
"volume": "374",
"year": "2016"
}
],
"reference-count": 94,
"references-count": 94,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9032/11/8/1192"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Health Information Management",
"Health Informatics",
"Health Policy",
"Leadership and Management"
],
"subtitle": [],
"title": "Clinical Disease Characteristics and Treatment Trajectories Associated with Mortality among COVID-19 Patients in Punjab, Pakistan",
"type": "journal-article",
"volume": "11"
}