Critical appraisal of multidrug therapy in the ambulatory management of patients with COVID-19 and hypoxemia
Eleftherios Gkioulekas, Peter A Mccullough, Colleen Aldous
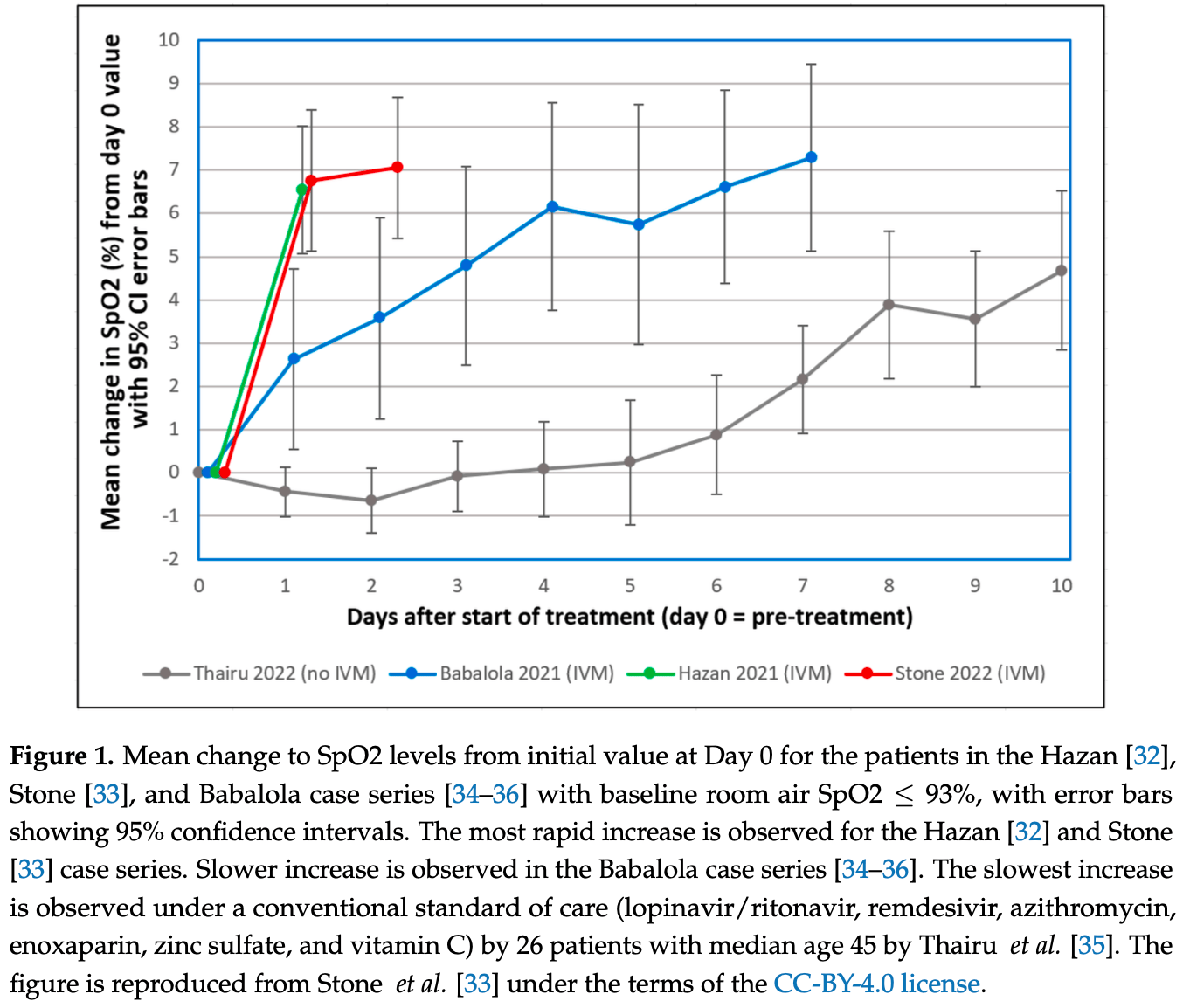
This critical appraisal is focused on three published case series of a total of 119 COVID-19 patients with hypoxemia who were successfully treated in the United States, Zimbabwe, and Nigeria with similar off-label multidrug treatments that may include ivermectin, nanosilver, doxycycline, zinc, and vitamins C and D, resulting in rapid recovery of oxygen levels. We investigate whether these treatment protocols were successful in preventing hospitalizations and deaths. We use a simplified self-controlled case series method to investigate the association of treatment with the existence of a hospitalization rate reduction effect. To show the association of treatment with the existence of a mortality rate reduction effect, we make conservative comparisons of the treatment case series with several external control groups using the exact Fisher test. A novel statistical technique, based on the Sterne interval and the Bayesian factor, is used to assess the resilience of these results with respect to selection bias. The existence of statistically significant hospitalization rate reduction is shown for two of the three case series with the most aggressive treatments, and it is resilient against both random and systemic selection bias. Combining all three case series allows us to show the existence of statistically significant mortality rate reduction, and it is more likely than not that random selection bias does not overturn this finding. These results, combined with an extensive literature review, show that the efficacy of these multidrug treatments is supported by the Bradford Hill criteria of strength of association, temporality, biological gradient, consistency, and biological plausibility.
Informed Consent Statement: Not applicable. The study is a analysis of previously published data.
Conflicts of Interest: The authors declare no conflict of interest.
Abbreviations The following abbreviations are used in this manuscript:
References
Adjei, Hong, Molinari, Bull-Otterson, Ajani et al., Mortality Risk Among Patients Hospitalized Primarily for COVID-19 During the Omicron and Delta Variant Pandemic Periods -United States, April 2020-June 2022, Morbidity and Mortality Weekly Report
Akinbolagbe, Otrofanowei, Akase, Akintan1, Ima-Edomwonyi et al., Predictors and outcomes of COVID-19 patients with hypoxemia in Lagos, Nigeria, Journal of the Pan African Thoracic Society
Almanza-Reyes, Moreno, Plascencia-Lopez, Alvarado-Vera, Patron-Romero et al., Evaluation of silver nanoparticles for the prevention of SARS-CoV-2 infection in health workers: In vitro and in vivo, PLoS ONE
Aminpour, Cannariato, Safaeeardebili, Preto, Moracchiato et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation
Annunziata, Coppola, Carannante, Simioli, Lanza et al., Home Management of Patients with Moderate or Severe Respiratory Failure Secondary to COVID-19, Using Remote Monitoring and Oxygen with or without HFNC, Pathogens
Arefin, Povidone Iodine (PVP-I) Oro-Nasal Spray: An Effective Shield for COVID-19 Protection for Health Care Worker (HCW), for all, Indian J Otolaryngol Head Neck Surg
Asghar, Yousuf, Shoaib, Asghar, Antibacterial, anticoagulant and cytotoxic evaluation of biocompatible nanocomposite of chitosan loaded green synthesized bioinspired silver nanoparticles, International Journal of Biological Macromolecules
Assoumou, Simmons, guidelines for hospital admission from the emergency department for patients with presumed or confirmed COVID-19
Babalola, Ajayi, Yunusa, Ndanusa, Ogedengbe et al., Ivermectin is Associated with Increase in SpO2 in Hypoxemic SARS-CoV-2 Patients: Pharmacodynamic Profile and Correlates, Journal of Clinical Chemistry and Laboratory Medicine
Babalola, Karu, None
Babalola, Ndanusa, Ajayi, Ogedengbe, Thairu et al., A Randomized Controlled Trial of Ivermectin Monotherapy versus Hydroxychloroquine, Ivermectin, and Azithromycin Combination Therapy in COVID-19 Patients in Nigeria, Journal of Infectious Diseases and Epidemiology
Bahl, Van Baalen, Ortiz, Chen, Todd et al., Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort, Internal and Emergency Medicine
Balmforth, Swales, Silpa, Dunton, Davies et al., Evaluating the efficacy and safety of a novel prophylactic nasal spray in the prevention of SARS-CoV-2 infection: A multi-centre, double blind, placebo-controlled, randomised trial, Journal of Clinical Virology
Basu, Khawaja, Rizvi, Sanchez-Gonzalez, Ferrer, Evaluation of Patient Experience for a Computationally-Guided Intranasal Spray Protocol to Augment Therapeutic Penetration: Implications for Effective Treatments for COVID-19, Rhinitis, and Sinusitis, Medical Research Archives,
doi:10.18103/mra.v10i4.2774Berger, Could Fisher, Jeffreys, and Neyman have agreed on testing, Statistical Science
Borody, Clancy, Combination therapy for COVID-19 based on ivermectin in an Australian population
Boschi, Scheim, Bancod, Militello, Bideau et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, International Journal of Molecular Sciences
Bramante, Huling, Tignanelli, Buse, Liebovitz et al., Randomized Trial of Metformin, Ivermectin, and Fluvoxamine for COVID-19, New England Journal of Medicine
Brouqui, Million, Parola, Mccullough, Raoult, Outcomes after early treatment with hydroxychloroquine and azithromycin: An analysis of a database of 30,423 COVID-19 patients, New Microbes and New Infections
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research
Castillejos-Lopez, Torres-Espindola, Huerta-Cruz, Flores-Soto, Romero-Martinez et al., Ivermectin: A Controversial Focal Point during the COVID-19 Pandemic, Life
Chamie, Hibberd, Scheim, COVID-19 Excess Deaths in Peru's 25 States in 2020: Nationwide Trends, Confounding Factors, and Correlations With the Extent of Ivermectin Treatment by State, Cureus
Chavez, Mcgee1, Mambie, Vallejo, Alonso et al., Team of work COVID-19 from Hospital Universitario Ramon y Cajal. COVID-19 hospital admission appropriateness analysis, American Journal of Biomedical Science and Research
Chen, Wu, Guo, Cao, Huang et al., Clinical and immunological features of severe and moderate coronavirus disease 2019, The Journal of Clinical Investigation
Chetty, Elucidating the pathogenesis and Rx of COVID reveals a missing element, Modern Medicine
Chitungo, Dzinamarira, Tungwarara, Chimene, Mukwenha et al., COVID-19 Response in Zimbabwe: The Need for a Paradigm Shift, COVID
Choudhury, Shabnam, Ahsan, Kabir, Khan et al., Effect of 1% Povidone Iodine Mouthwash/Gargle, Nasal and Eye Drop in COVID-19 patient, Bioresearch Communications -(BRC)
Clinic, Cleveland Clinic admission guidelines for confirmed or suspected COVID-19 patients
Core, R: A Language and Environment for Statistical Computing
Dayyab, Bashir, Sulaiman, Iliyasu, Hamza et al., Determinants of mortality among hospitalized patients with COVID-19 during first and second waves of the pandemic: A retrospective cohort study from an isolation center in Kano, Nigeria, PLoS ONE
Derouiche, Chetehouna, Djouadi, Boulaares, Guemari, The Possible Mechanisms of Silver Nanoparticles against Sars-CoV 2, Frontiers in Biomedical Technologies
Derwand, Scholz, Zelenko, COVID-19 outpatients -Early risk-stratified treatment with zinc plus low dose hydroxychloroquine and azithromycin: A retrospective case series study, International Journal of Antimicrobial Agents
Fazio, Bellavite, Zanolin, Mccullough, Pandolfi et al., Retrospective Study of Outcomes and Hospitalization Rates of Patients in Italy with a Confirmed Diagnosis of Early COVID-19 and Treated at Home Within 3 Days or After 3 Days of Symptom Onset with Prescribed and Non-Prescribed Treatments Between November 2020 and August 2021, Medical Science Monitor
Fedak, Bernal, Capshaw, Gross, Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology, Emerging Themes in Epidemiology
Garza-Santiago, Ortiz-Hernandez, Kammar-Garcia, Mancilla-Galindo, Comment on: 'Effectiveness of ivermectinbased multidrug therapy in severely hypoxic, ambulatory COVID-19 patients, Future Microbiology
Gautret, Lagier, Parola, Hoang, Meddeb et al., Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial, International Journal of Antimicrobial Agents
Gkioulekas, Mccullough, Zelenko, Statistical analysis methods applied to early outpatient COVID-19 treatment case series data, COVID
Gkioulekas, Supplementary material: Critical appraisal of multi-drug therapy in the ambulatory management of patients with COVID-19 and hypoxemia,
doi:10.6084/m9.figshare.24329611Goodman, Toward evidence-based medical statistics. 1: The P value fallacy, Annals of Internal Medicine
Goodman, Toward evidence-based medical statistics. 2: The Bayes factor, Annals of Internal Medicine
Guzzo, Furtek, Porras, Chen, Tipping et al., Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects, Journal of Clinical Pharmacology
Hamadeh, Van Rompaey, Metreau, Eapen, New World Bank country classifications by income level: 2022-2023
Hazan, Dave, Gunaratne, Dolai, Clancy et al., Effectiveness of ivermectin-based multidrug therapy in severely hypoxic, ambulatory COVID-19 patients, Future Microbiology
Hazan, Dave, Mccullough, Borody, Letter in reply: more power to ivermectin multidrug therapy, Future Microbiology
Hazan, None
Hill, The Environment and Disease: Association or Causation?, Proceedings of the Royal Society of Medicine
Huijghebaert, Parviz, Rabago, Baxter, Chatterjee et al., Saline nasal irrigation and gargling in COVID-19: a multidisciplinary review of effects on viral load, mucosal dynamics, and patient outcomes, Frontiers in Public Health
Jassat, Mudara, Ozougwu, Tempia, Blumberg et al., Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: A cohort study, Lancet Global Health
Jeremiah, Miyakawa, Morita, Yamaoka, Ryo, Potent antiviral effect of silver nanoparticles on SARS-CoV-2, Biochemical and Biophysical Research Communications
Karim, Devnarain, Time to Stop Using Ineffective Covid-19 Drugs, New England Journal of Medicine
Kass, Raftery, Bayes Factors, Journal of the American Statistical Association
Kerr, Baldi, Lobo, Assagra, Proenca et al., Regular Use of Ivermectin as Prophylaxis for COVID-19 Led Up to a 92% Reduction in COVID-19 Mortality Rate in a Dose-Response Manner: Results of a Prospective Observational Study of a Strictly Controlled Population of 88,012 Subjects, Cureus
Kerr, Cadegiani, Baldi, Lobo, Assagra et al., Ivermectin prophylaxis used for COVID-19 reduces COVID-19 infection and mortality rates: A 220,517-subject, populational-level retrospective citywide, Cureus
Knight, Ho, Pius, Buchan, Carson et al., Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: Development and validation of the 4C Mortality Score, BMJ
Kory, Meduri, Iglesias, Varon, Cadegiani et al., MATH+ Multi-Modal Hospital Treatment Protocol for COVID-19 Infection: Clinical and Scientific Rationale, Journal of Clinical Medicine Research
Kouamou, Matarise, Santos, Elose, Manasa, SARS-CoV-2 in Zimbabwe: Milestones and challenges faced towards achieving the expected 60% herd immunity, Pan African Medical Journal
Lehrer, Rheinstein, Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, Vivo
Lim, Hor, Tay, Jelani, Tan et al., Efficacy of ivermectin treatment on disease progression among adults with mild to moderate COVID-19 and comorbidities: The I-TECH randomized clinical trial, JAMA Internal Medicine
Lima-Morales, Mendez-Hernandez, Flores, Osorno-Romero, Sancho-Hernandez et al., Effectiveness of a multidrug therapy consisting of Ivermectin, Azithromycin, Montelukast, and Acetylsalicylic acid to prevent hospitalization and death among ambulatory COVID-19 cases in Tlaxcala, Mexico, International Journal of Infectious Diseases
Lopez-Medina, Lopez, Hurtado, Davalos, Ramirez et al., Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: A randomized clinical trial, Journal of the American Medical Association
Madamombe, Shambira, Masoja, Dhliwayo, Juru et al., Factors associated with COVID-19 fatality among patients admitted in Mashonaland West Province, Zimbabwe 2020-2022: A secondary data analysis, Pan African Medical Journal
Mahmud, Rahman, Alam, Ahmed, Kabir et al., Ivermectin in combination with doxycycline for treating COVID-19 symptoms: a randomized trial, Journal of International Medical Research
Malek, Granwehr, Kontoyiannis, Doxycycline as a potential partner of COVID-19 therapies, IDCases
Marik, Kory, Varon, Iglesias, Meduri, MATH+ protocol for the treatment of SARS-CoV-2 infection: the scientific rationale, Expert Review of Anti-infective Therapy
Mathieu, Ritchie, Rodes-Guirao, Appel, Giattino et al., The Place of Ivermectin in the Management of Covid-19: State of the Evidence, Medical Research Archives,
doi:10.18103/mra.v11i4.3778.105Maxima, Maxima, None, a Computer Algebra System
Mccullough, Alexander, Armstrong, Arvinte, Bain et al., Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19), Reviews in Cardiovascular Medicine
Mccullough, Innovative Early Sequenced Multidrug Therapy for SARS-CoV-2 (COVID-19) Infection to Reduce Hospitalization and Death, International Journal of Medical Science and Clinical invention
Mccullough, Kelly, Ruocco, Lerma, Tumlin et al., Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection, The American Journal of Medicine
Mccullough, Oskoui, Early multidrug regimens in new potentially fatal medical problems, Reviews in Cardiovascular Medicine
Mcgonagle, Bridgewood, Meaney, A tricompartmental model of lung oxygenation disruption to explain pulmonary and systemic pathology in severe COVID-19, Lancet Respiratory Medicine
Mejia, Medina, Cornejo, Morello, Vasquez et al., Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru, PLoS ONE
Miklowski, Jansen, Auron, Whinney, The hospitalized patient with COVID-19 on the medical ward: Cleveland Clinic approach to management, Cleveland Clinical Journal of Medicine,
doi:10.3949/ccjm.87a.ccc064Miller, Tada, Goto, Chen, Dang et al., Prediction models for severe manifestations and mortality due to COVID-19: A systematic review, Academic Emergency Medicine
Million, Lagier, Tissot-Dupont, Ravaux, Dhiver et al., Early Treatment with Hydroxychloroquine and Azithromycin in 10,429 COVID-19 Outpatients: A Monocentric Retrospective Cohort Study, Reviews in Cardiovascular Medicine
Morey, Romeijn, Rouder, The philosophy of Bayes factors and the quantification of statistical evidence, Journal of Mathematical Psychology
Murchu, Byrne, Carty, Gascun, Keogan et al., Quantifying the risk of SARS-CoV-2 reinfection over time, Reviews in Medical Virology
Naggie, Boulware, Lindsell, Stewart, Gentile et al., Effect of Ivermectin vs. Placebo on Time to Sustained Recovery in Outpatients With Mild to Moderate COVID-19: A Randomized Clinical Trial, Journal of the American Medical Association
Naggie, Boulware, Lindsell, Stewart, Slandzicki et al., Effect of Higher-Dose Ivermectin for 6 Days vs. Placebo on Time to Sustained Recovery in Outpatients With COVID-19: A Randomized Clinical Trial, Journal of the American Medical Association
Nardo, Gentilotti, Mazzaferri, Cremonini, Hansen et al., the members of the COVID-19MCDA Group. Multi-Criteria Decision Analysis to prioritize hospital admission of patients affected by COVID-19 in low-resource settings with hospital-bed shortage, International Journal of Infectious Diseases
Osman, Farouk, Osman, Abdrabou, Longitudinal assessment of chest computerized tomography and oxygen saturation for patients with COVID-19, The Egyptian Journal of Radiology and Nuclear Medicine
Palazzuoli, Beltrami, Mccullough, Acute COVID-19 Management in Heart Failure Patients: A Specific Setting Requiring Detailed Inpatient and Outpatient Hospital Care, Biomedicines
Petersen, Douglas, Whitaker, Self controlled case series methods: an alternative to standard epidemiological study designs, BMJ
Pilaquinga, Morey, Torres, Seqqat, Pina, Silver nanoparticles as a potential treatment against SARS-CoV-2: A review, Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology
Poskurica, Stevanovic, Zdravkovic, Cekerevac, Cupurdija et al., Admission Predictors of Mortality in Hospitalized COVID-19 Patients-A Serbian Cohort Study, Journal of Clinical Medicine
Prabhakaran, Singh, Kondal, Raspail, Mohan et al., Cardiovascular Risk Factors and Clinical Outcomes among Patients Hospitalized with COVID-19: Findings from the World Heart Federation COVID-19 Study, Global Heart
Procter, Ross, Pickard, Smith, Hanson et al., Clinical outcomes after early ambulatory multidrug therapy for high-risk SARS-CoV-2 (COVID-19) infection, Reviews in Cardiovascular Medicine
Procter, Ross, Pickard, Smith, Hanson et al., Early Ambulatory Multidrug Therapy Reduces Hospitalization and Death in High-Risk Patients with SARS-CoV-2 (COVID-19), International Journal of Innovative Research in Medical Science
Rajter, Sherman, Fatteh, Vogel, Sacks et al., Use of Ivermectin Is Associated With Lower Mortality in Hospitalized Patients With Coronavirus Disease, CHEST
Reina, Peng, Jacquemin, Andrade, Bianco, Hard nanomaterials in time of viral pandemics, ACS Nano
Reis, Silva, Silva, Thabane, Milagres et al., Effect of early treatment with ivermectin among patients with COVID-19, New England Journal of Medicine
Rendell, Commentary on 'Statistical Analysis Methods Applied to Early Outpatient COVID-19 Treatment Case Series Data' by Gkioulekas, McCullough and Zelenko: A Return Back to the Future, Journal of Healthcare Communications
Risch, Early Outpatient Treatment of Symptomatic, High-Risk COVID-19 Patients that Should be Ramped-Up Immediately as Key to the Pandemic Crisis, American Journal of Epidemiology
Rizzo, Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action, Naunyn-Schmiedeberg's Archives of Pharmacology
Santin, Scheim, Mccullough, Yagisawa, Borody, Ivermectin: a multifaceted drug of Nobel prize-honoured distinction with indicated efficacy against a new global scourge, COVID-19, New Microbes and New Infections
Scheim, A Deadly Embrace: Hemagglutination Mediated by SARS-CoV-2 Spike Protein at Its 22 N-Glycosylation Sites, Red Blood Cell Surface Sialoglycoproteins, and Antibody, International Journal of Molecular Sciences
Scheim, Aldous, Osimani, Fordham, Hoy, When Characteristics of Clinical Trials Require Per-Protocol as Well as Intention-To-Treat Outcomes to Draw Reliable Conclusions: Three Examples, Journal of Clinical Medicine
Scheim, Hibberd, Chamie-Quintero, Protocol violations in Lopez-Medina et al.: 38 switched ivermectin (IVM) and placebo doses, failure of blinding, widespread IVM sales OTC in Cali, and nearly identical AEs for the IVM and control groups,
doi:10.31219/osf.io/u7ewzSoler, De Mendoza, Cuello, Silva-Vetri, Nunez et al., Intranasal Xylitol for the Treatment of COVID-19 in the Outpatient Setting: A Pilot Study, Cureus
Sterne, Some remarks on confidence or fiducial limits, Biometrika
Stone, Gill, Zimbabwe SID Protocol
Stone, Ndarukwa, Scheim, Dancis, Dancis et al., Changes in SpO2 on Room Air for 34 Severe COVID-19 Patients after Ivermectin-Based Combination Treatment: 62% Normalization within 24 Hours, Biologics
Stone, Ndarukwa, Scheim, Dancis, Dancis et al., Rapid increase of SpO2 on room air for 34 severe COVID-19 patients after ivermectin-based combination treatment: 55-62% normalization within 12-24 hours,
doi:10.21203/rs.3.rs-1048271/v1Thairu, Babalola, Ajayi, Ndanusa, Ogedengbe et al., A Comparison of Ivermectin and Non Ivermectin Based Regimen for COVID-19 in Abuja: Effects on Virus Clearance, Days-to-discharge and Mortality, Journal of Pharmaceutical Research International
Tran, Pham, Nguyen, Tran, Hoang et al., Therapeutic Efficacy of AFree Oral Spray on the Symptoms and Course of Moderate and Severe COVID-19 in the Field Hospital, In Vivo
Trejo, Castaneda, Rodriguez, Carmona, Mercado et al., Hydrogen Peroxide as an Adjuvant Therapy for COVID-19: A Case Series of Patients and Caregivers in the Mexico City Metropolitan Area, Evidence-based Complementary and Alternative Medicine
Tyson, Fareed, Overcoming the Covid darkness, How two doctors successfully treated
Wessels, Rolles, Rink, The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis, Frontiers in Immunology
Wong, Viswanathan, Wang, Sun, Clark et al., Current and future developments in the treatment of virus-induced hypercytokinemia, Future Medicinal Chemistry
Xu, Tang, Liu, Wang, Liu, Evaluation of the adjuvant effect of silver nanoparticles both in vitro and in vivo, Toxicology Letters
Yagisawa, Foster, Hanaki, Omura, Global trends in novel coronavirus infection (COVID-19) and its treatment-Analyses of the background of ivermectin clinical trial, The Japanese Journal of Antibiotics
Yates, Newman, Oshry, Glassman, Leone et al., Doxycycline treatment of high-risk COVID-19-positive patients with comorbid pulmonary disease, Therapeutic Advances in Respiratory Disease
Zachar, Nanomedicine formulations for respiratory infections by inhalation delivery: Covid-19 and beyond, Medical Hypotheses
Zaidi, Dehgani-Mobaraki, The mechanisms of action of ivermectin against SARS-CoV-2. An extensive review, The Journal of Antibiotics
Zbarsky, Thomas, Greenfield, Bioactivity of a peptide derived from acetylcholinesterase: involvement of an ivermectinsensitive site on the alpha 7 nicotinic receptor, Neurobiology of Disease