COVID-19: Unveiling the Neuropsychiatric Maze—From Acute to Long-Term Manifestations
Daniela Ariza, Lily Castellar-Visbal, Maria Marquina, Diego Rivera-Porras, Nestor Galbán, Raquel Santeliz, Melissa Gutiérrez-Rey, Heliana Parra, José Vargas-Manotas, Wheeler Torres, Laura Quintana-Espinosa, Alexander Manzano, Lorena Cudris-Torres, Valmore Bermúdez
Biomedicines, doi:10.3390/biomedicines12061147
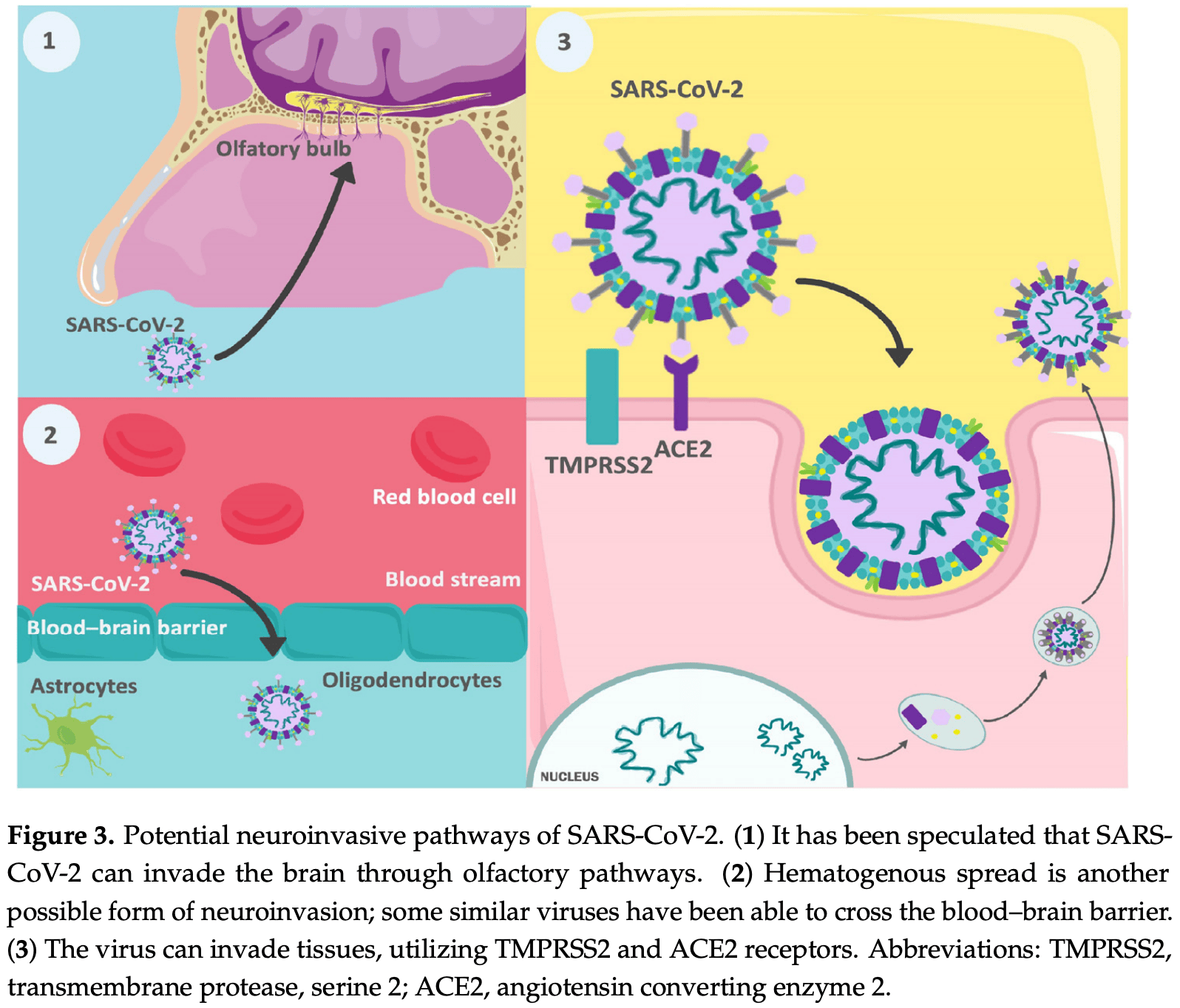
The SARS-CoV-2 virus has spread rapidly despite implementing strategies to reduce its transmission. The disease caused by this virus has been associated with a diverse range of symptoms, including common neurological manifestations such as dysgeusia, anosmia, and myalgias. Additionally, numerous cases of severe neurological complications associated with this disease have been reported, including encephalitis, stroke, seizures, and Guillain-Barré syndrome, among others. Given the high prevalence of neurological manifestations in this disease, the objective of this review is to analyze the mechanisms by which this virus can affect the nervous system, from its direct invasion to aberrant activation of the immune system and other mechanisms involved in the symptoms, including neuropsychiatric manifestations, to gain a better understanding of the disease and thus facilitate the search for effective therapeutic strategies.
Conflicts of Interest: The authors declare no conflicts of interest.
References
Abdelhady, Husain, Hawas, Elazb, Mansour et al., Encephalitis following COVID-19 Vaccination: A Systematic Review, Vaccines,
doi:10.3390/vaccines11030576Ahmed, Ahmad, Hassan, Kakamad, Salih et al., Post COVID-19 neurological complications; a meta-analysis, Ann. Med. Surg,
doi:10.1016/j.amsu.2022.103440Ahmed, Hanif, Ali, Haider, Kherani et al., Neurological manifestations of COVID-19 (SARS-CoV-2): A review, Front. Neurol,
doi:10.3389/fneur.2020.00518Al-Aly, Rosen, Long Covid and Impaired Cognition-More Evidence and More Work to Do, N. Engl. J. Med,
doi:10.1056/NEJMe2400189Al-Husinat, Nusir, Al-Gharaibeh, Alomari, Smadi et al., Post-COVID-19 syndrome symptoms after mild and moderate SARS-CoV-2 infection, Front. Med,
doi:10.3389/fmed.2022.1017257Alberti, Beretta, Piatti, Karantzoulis, Piatti et al., Guillain-Barré syndrome related to COVID-19 infection, Neurol. Neuroimmunol. Neuroinflamm,
doi:10.1212/NXI.0000000000000741Alketbi, Alnuaimi, Almulla, Altalai, Samir et al., Acute myelitis as a neurological complication of Covid-19: A case report and MRI findings, Radiol. Case Rep,
doi:10.1016/j.radcr.2020.06.001Allahyari, Molaee, Nejad, COVID-19 vaccines and neurological complications: A systematic review, Zeitschrift fur Naturforschung. J. Biosci
Antinone, Smith, Retrograde axon transport of herpes simplex virus and pseudorabies virus: A live-cell comparative analysis, J. Virol,
doi:10.1128/JVI.02029-09Arabi, Harthi, Hussein, Bouchama, Johani et al., Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV), Infection,
doi:10.1007/s15010-015-0720-yAydin, Özdemir, Gündüz, Kiziltan, Seizures in patients with respiratory disease-A retrospective single center study, Arq. Neuro-Psiquiatr,
doi:10.1590/0004-282x20190196Bernard-Valnet, Pizzarotti, Anichini, Demars, Russo et al., Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection, Eur. J. Neurol,
doi:10.1111/ene.14298Beyrouti, Adams, Benjamin, Cohen, Farmer et al., Characteristics of ischaemic stroke associated with COVID-19, J. Neurol. Neurosurg. Psychiatry,
doi:10.1136/jnnp-2020-323586Bonetto, Pasetto, Lisi, Carbonara, Zangari et al., Markers of blood-brain barrier disruption increase early and persistently in COVID-19 patients with neurological manifestations, Front. Immunol,
doi:10.3389/fimmu.2022.1070379Boss, Seegmiller, Age-related physiological changes and their clinical significance, West. J. Med
Braga, Lepra, Kish, Rusjan, Nasser et al., Neuroinflammation After COVID-19 with Persistent Depressive and Cognitive Symptoms, JAMA Psychiatry,
doi:10.1001/jamapsychiatry.2023.1321Brann, Tsukahara, Weinreb, Lipovsek, Van Den Berge et al., Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia, Sci. Adv,
doi:10.1126/sciadv.abc5801Bullen, Hogberg, Bahadirli-Talbott, Bishai, Hartung et al., Infectability of human BrainSphere neurons suggests neurotropism of SARS-CoV-2, ALTEX
Caamaño, Beato, Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2, J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas
Castanares-Zapatero, Chalon, Kohn, Dauvrin, Detollenaere et al., Pathophysiology and mechanism of long COVID: A comprehensive review, Ann. Med,
doi:10.1080/07853890.2022.2076901Chan, Chan, Choi, To, Tse et al., Differential cell line susceptibility to the emerging novel human betacoronavirus 2c EMC/2012: Implications for disease pathogenesis and clinical manifestation, J. Infect. Dis,
doi:10.1093/infdis/jit123Chan, Ebadi, Sarna, Guillain-Barré Syndrome with Facial Diplegia Related to SARS-CoV-2 Infection, Can. J. Neurol. Sci. J. Can. Sci. Neurol,
doi:10.1017/cjn.2020.106Ciolac, Crivorucica, Zota, Gorincioi, Efremova et al., Extensive cerebellar involvement and cognitive impairment in COVID-19-associated acute necrotizing encephalopathy, Ther. Adv. Neurol. Disord,
doi:10.1177/1756286420985175Da Costa, Rato, Cruz, Valadas, Antunes et al., Longitudinally extensive transverse myelitis with anti-myelin oligodendrocyte glycoprotein antibodies following SARS-CoV-2 infection, J. Neuroimmunol,
doi:10.1016/j.jneuroim.2021.577739Dalakas, Guillain-Barré syndrome: The first documented COVID-19-triggered autoimmune neurologic disease: More to come with myositis in the offing, Neurol. Neuroimmunol. Neuroinflamm,
doi:10.1212/NXI.0000000000000781Davis, Mccorkell, Vogel, Topol, Long COVID: Major findings, mechanisms and recommendations, Nature reviews. Microbiology
Delamarre, Grouteau, Rousset, Jimena, Roustan et al., COVID-19 related acute necrotizing encephalopathy with extremely high interleukin-6 and RANBP2 mutation in a patient with recently immunized inactivated virus vaccine and no pulmonary involvement, J. Neurol. Neurosurg. Psychiatry,
doi:10.1186/s12879-022-07610-0Desforges, Le Coupanec, Dubeau, Bourgouin, Lajoie et al., Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System?, Viruses,
doi:10.3390/v12010014Diaz, Bueno, Zeas, Klinger, Núñez et al., Estatus epiléptico en niños: Aspectos generales diagnósticos y terapéuticos, Arch. Venez. Farmacol. Ter
Dietsch, Solomon, Steele, Pelletier, The effect of barium on perceptions of taste intensity and palatability, Dysphagia,
doi:10.1007/s00455-013-9487-4Dixon, Varley, Gontsarova, Mallon, Tona et al., COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia, Neurol. Neuroimmunol. Neuroinflamm,
doi:10.1212/NXI.0000000000000789Dubé, Le Coupanec, Wong, Rini, Desforges et al., Axonal Transport Enables Neuron-to-Neuron Propagation of Human Coronavirus OC43, J. Virol,
doi:10.1128/JVI.00404-18El Otmani, El Moutawakil, Rafai, El Benna, El Kettani et al., Covid-19 and Guillain-Barré syndrome: More than a coincidence!, Rev. Neurol,
doi:10.1016/j.neurol.2020.04.007Farzi, Ayromlou, Jahanbakhsh, Bavil, Janzadeh et al., Guillain-Barré syndrome in a patient infected with SARS-CoV-2, a case report, J. Neuroimmunol,
doi:10.1016/j.jneuroim.2020.577294Ferrando, Klepacz, Lynch, Tavakkoli, Dornbush et al., COVID-19 Psychosis: A Potential New Neuropsychiatric Condition Triggered by Novel Coronavirus Infection and the Inflammatory Response?, Psychosomatics,
doi:10.1016/j.psym.2020.05.012Flannery, Yang, Keyvani, Sakoulas, Acute Psychosis Due to Anti-N-Methyl D-Aspartate Receptor Encephalitis Following COVID-19 Vaccination: A Case Report, Front. Neurol,
doi:10.3389/fneur.2021.764197Giannis, Ziogas, Gianni, Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past, J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol,
doi:10.1016/j.jcv.2020.104362Gombolay, Hallman-Cooper, COVID-19 and the Pandemic-Related Aspects in Pediatric Demyelinating Disorders, Semin. Pediatr. Neurol,
doi:10.1016/j.spen.2023.101055González-González, Actualidades en la fisiopatología del trastorno por estrés postraumático (TEPT), Salud Jalisco
González-González, Arvilla-Arce, Alteraciones neuropsiquiátricas de la enfermedad por COVID-19
Gorbalenya, Baker, Baric, De Groot, Drosten et al., The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2, Nat. Microbiol
Gutiérrez-Ortiz, Méndez-Guerrero, Rodrigo-Rey, Pedro-Murillo, Bermejo-Guerrero et al., Miller Fisher syndrome and polyneuritis cranialis in COVID-19, Neurology,
doi:10.1212/WNL.0000000000009619Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, J. Pathol,
doi:10.1002/path.1570Hampshire, Azor, Atchison, Trender, Hellyer et al., Cognition and Memory after Covid-19 in a Large Community Sample, N. Engl. J. Med,
doi:10.1056/NEJMoa2311330Haroun, Dieiev, Kang, Barbi, Nia et al., Rhabdomyolysis in COVID-19 Patients: A Retrospective Observational Study, Cureus,
doi:10.7759/cureus.12552Helms, Kremer, Merdji, Clere-Jehl, Schenck et al., Neurologic Features in Severe SARS-CoV-2 Infection, N. Engl. J. Med,
doi:10.1056/NEJMc2008597Helms, Tacquard, Severac, Leonard-Lorant, Ohana et al., High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study, Intensive Care Med,
doi:10.1007/s00134-020-06062-xHoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, Cell,
doi:10.1016/j.cell.2020.02.052Hou, Li, Yoon, Leung, You et al., Enhanced replication of SARS-CoV-2 Omicron BA.2 in human forebrain and midbrain organoids, Signal Transduct. Target. Ther,
doi:10.1038/s41392-022-01241-2Hussaini, Rogers, Kataria, Uddin, Mohamed et al., COVID-19-Induced Seizures: A Meta-Analysis of Case Series and Retrospective Cohorts, Cureus,
doi:10.7759/cureus.28633Jaunmuktane, Mahadeva, Green, Sekhawat, Barrett et al., Microvascular injury and hypoxic damage: Emerging neuropathological signatures in COVID-19, Acta Neuropathol,
doi:10.1007/s00401-020-02190-2Jomaa, El Halabi, Melhem, Dib, Ghosn et al., COVID-19-Associated Acute Asymmetric Hemorrhagic Necrotizing Encephalopathy: A Case Report, Neurohospitalist,
doi:10.1177/19418744211055360Kanberg, Ashton, Andersson, Yilmaz, Lindh et al., Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19, Neurology,
doi:10.1212/WNL.0000000000010111Karimi, Razavi, Rouhani, Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report, Iran. Red. Crescent Med. J,
doi:10.5812/ircmj.102828Khair, Nikam, Husain, Ortiz, Kaur, Para and Post-COVID-19 CNS Acute Demyelinating Disorders in Children: A Case Series on Expanding the Spectrum of Clinical and Radiological Characteristics, Cureus,
doi:10.7759/cureus.23405Kim, Chung, Jo, Lee, Kim et al., Identification of Coronavirus Isolated from a Patient in Korea with COVID-19, Osong Public Health Res. Perspect,
doi:10.24171/j.phrp.2020.11.1.02Lazarte-Rantes, Guevara-Castañón, Romero, Guillén-Pinto, Acute Necrotizing Encephalopathy Associated with SARS-CoV-2 Exposure in a Pediatric Patient, Cureus,
doi:10.7759/cureus.15018Lechien, Chiesa-Estomba, De Siati, Horoi, Le Bon et al., Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study, Eur. Arch. Oto-Rhino-Laryngol,
doi:10.1007/s00405-020-05965-1Lee, Min, Lee, Kim, Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients, J. Korean Med. Sci,
doi:10.3346/jkms.2020.35.e174Leng, Shah, Ahmad, Premraj, Bassi et al., Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics, Cells,
doi:10.3390/cells12050816Li, Li, Fan, Wen, Zhang et al., Coronavirus Infections in the Central Nervous System and Respiratory Tract Show Distinct Features in Hospitalized Children, Intervirology,
doi:10.1159/000453066Li, Li, Wang, Zhou, Chang et al., Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study, Stroke Vasc. Neurol,
doi:10.1136/svn-2020-000431Lotan, Nishiyama, Manzano, Lydston, Levy, COVID-19 and the risk of CNS demyelinating diseases: A systematic review, Front. Neurol,
doi:10.3389/fneur.2022.970383Macgibeny, Koyuncu, Wirblich, Schnell, Enquist, Retrograde axonal transport of rabies virus is unaffected by interferon treatment but blocked by emetine locally in axons, PLoS Pathog,
doi:10.1371/journal.ppat.1007188Mao, Chen, He, Chang, Hong et al., Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study, MedRxiv,
doi:10.1001/jamaneurol.2020.1127Mao, Jin, Wang, Hu, Chen et al., Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China, JAMA Neurol,
doi:10.1001/jamaneurol.2020.1127Marenco, Lozada, Unusual Clinical Presentation of Guillain Barre Syndrome: A Case Report
Mccarthy, Wilczynski, Wenceslau, Webb, A new storm on the horizon in COVID-19: Bradykinin-induced vascular complications, Vasc. Pharmacol,
doi:10.1016/j.vph.2020.106826Medetalibeyoglu, Kaytaz, Senkal, Genc, Aktar et al., Would Tracking Coagulation Together with Inflamation Markers be a Prospect for COVID-19 Disease Prognosis?, Clin. Lab,
doi:10.7754/Clin.Lab.2021.210802Meinhardt, Radke, Dittmayer, Franz, Thomas et al., Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19, Nat. Neurosci,
doi:10.1038/s41593-020-00758-5Mesci, De Souza, Martin-Sancho, Macia, Saleh et al., SARS-CoV-2 infects human brain organoids causing cell death and loss of synapses that can be rescued by treatment with Sofosbuvir, PLoS Biol,
doi:10.1371/journal.pbio.3001845Milanetti, Miotto, Di Rienzo, Nagaraj, Monti et al., In-Silico Evidence for a Two Receptor Based Strategy of SARS-CoV-2, Front. Mol. Biosci,
doi:10.3389/fmolb.2021.690655Moriguchi, Harii, Goto, Harada, Sugawara et al., A first case of meningitis/encephalitis associated with SARS-Coronavirus-2, Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis,
doi:10.1016/j.ijid.2020.03.062Mullaguri, Sivakumar, Battineni, Anand, Vanderwerf, COVID-19 Related Acute Hemorrhagic Necrotizing Encephalitis: A Report of Two Cases and Literature Review, Cureus,
doi:10.7759/cureus.14236Nampoothiri, Sauve, Ternier, Fernandois, Coelho et al., The hypothalamus as a hub for putative SARS-CoV-2 brain infection,
doi:10.1101/2020.06.08.139329Nandan, Sharma, Nandolia, Saxena, Verma, Acute Hemorrhagic Necrotizing Encephalopathy in Patients with COVID-19, Ann. Indian Acad. Neurol
Netland, Meyerholz, Moore, Cassell, Perlman, Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2, J. Virol,
doi:10.1128/JVI.00737-08Nguyen, Taylor, Guillain-Barre Syndrome, I
Niazkar, Zibaee, Nasimi, Bahri, The neurological manifestations of COVID-19: A review article, Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol,
doi:10.1007/s10072-020-04486-3Otani, Fukushima, Matsuishi, COVID-19 delirium and encephalopathy: Pathophysiology assumed in the first 3 years of the ongoing pandemic, Brain Disord,
doi:10.1016/j.dscb.2023.100074Ottaviani, Boso, Tranquillini, Gapeni, Pedrotti et al., Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): A case report from an Italian COVID-hospital, Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol,
doi:10.1007/s10072-020-04449-8Pamies, Barreras, Block, Makri, Kumar et al., A human brain microphysiological system derived from induced pluripotent stem cells to study neurological diseases and toxicity, ALTEX,
doi:10.14573/altex.1609122Panariello, Cellini, Speciani, De Ronchi, Atti, How Does SARS-CoV-2 Affect the Central Nervous System? A Working Hypothesis, Front. Psychiatry,
doi:10.3389/fpsyt.2020.582345Panigada, Bottino, Tagliabue, Grasselli, Novembrino et al., ypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis, J. Thromb. Haemost. JTH,
doi:10.1111/jth.14850Paniz-Mondolfi, Bryce, Grimes, Gordon, Reidy et al., Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), J. Med. Virol,
doi:10.1002/jmv.25915Patil, Patil, Gondhali, Toshniwal, Immune Dysregulation during and after COVID-19, Situation. J. Transl. Crit. Care Med,
doi:10.1097/JTCCM-D-22-00024Perumal, Shunmugam, Naidoo, Karim, Wilkins et al., Long COVID: A review and proposed visualization of the complexity of long COVID, Front. Immunol,
doi:10.3389/fimmu.2023.1117464Petrilli, Jones, Yang, Rajagopalan, O'donnell et al., Factors associated with hospitalization and critical illness among 4103 patients with COVID-19 disease in New York City,
doi:10.1101/2020.04.08.20057794Pilotto, Odolini, Masciocchi, Comelli, Volonghi et al., Steroid-Responsive Encephalitis in Coronavirus Disease, Ann. Neurol,
doi:10.1002/ana.25783Politi, Grimaldi, Magnetic Resonance Imaging Alteration of the Brain in a Patient With Coronavirus Disease 2019 (COVID-19) and Anosmia, JAMA Neurol,
doi:10.1001/jamaneurol.2020.2125Poyiadji, Shahin, Noujaim, Stone, Patel et al., COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features, Radiology,
doi:10.1148/radiol.2020201187Proust, Queval, Harvey, Adams, Bennett et al., Differential effects of SARS-CoV-2 variants on central nervous system cells and blood-brain barrier functions, J. Neuroinflamm,
doi:10.1186/s12974-023-02861-3Puelles, Lütgehetmann, Lindenmeyer, Sperhake, Wong et al., Multiorgan and Renal Tropism of SARS-CoV-2, N. Engl. J. Med,
doi:10.1056/NEJMc2011400Qi, Zhou, Hua, Zhang, Bian et al., The scRNA-seq Expression Profiling of the Receptor ACE2 and the Cellular Protease TMPRSS2 Reveals Human Organs Susceptible to SARS-CoV-2 Infection, Int. J. Environ. Res. Public Health,
doi:10.3390/ijerph18010284Reichard, Kashani, Boire, Constantopoulos, Guo et al., Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology, Acta Neuropathol,
doi:10.1007/s00401-020-02166-2Roche, Roche, A hypothesized role for dysregulated bradykinin signaling in COVID-19 respiratory complications, FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol,
doi:10.1096/fj.202000967Rodrigues, Dias, Paranhos, Silva, Bastos et al., Headache in long COVID as disabling condition: A clinical approach, Front. Neurol,
doi:10.3389/fneur.2023.1149294Rodriguez-Morales, Lopez-Echeverri, Perez-Raga, Quintero-Romero, Valencia-Gallego et al., The global challenges of the long COVID-19 in adults and children, Travel. Med. Infect. Dis,
doi:10.1016/j.tmaid.2023.102606Rogers, Chesney, Oliver, Pollak, Mcguire et al., Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic, Lancet Psychiatry,
doi:10.1016/S2215-0366(20)30203-0Rong-Hui, Li-Rong, Cheng-Qing, Wen, Tan-Ze et al., Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study, Eur. Respir. J
Rossi, Delsante, Pilato, Gnetti, Gabrielli et al., Kidney Biopsy Findings in a Critically Ill COVID-19 Patient with Dialysis-Dependent Acute Kidney Injury: A Case against "SARS-CoV-2 Nephropathy, Kidney Int. Rep,
doi:10.1016/j.ekir.2020.05.005Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med,
doi:10.1007/s00134-020-05991-xSadock, Sadock, Ruiz, Kaplan Y Sadock, Manual de Psiquiatría Clínica
Sankowski, Mader, Valdés-Ferrer, Systemic inflammation and the brain: Novel roles of genetic, molecular, and environmental cues as drivers of neurodegeneration, Front. Cell. Neurosci,
doi:10.3389/fncel.2015.00028Scheidl, Canseco, Hadji-Naumov, Bereznai, Guillain-Barré syndrome during SARS-CoV-2 pandemic: A case report and review of recent literature, J. Peripher. Nerv. Syst. JPNS,
doi:10.1111/jns.12382Schulte, Hauer, Kunz, Sellner, Systematic review of cases of acute myelitis in individuals with COVID-19, Eur. J. Neurol,
doi:10.1111/ene.14952Sedaghat, Karimi, Guillain Barre syndrome associated with COVID-19 infection: A case report, J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas,
doi:10.1016/j.jocn.2020.04.062Sidarta-Oliveira, Jara, Ferruzzi, Skaf, Velander et al., SARS-CoV-2 receptor is co-expressed with elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cell, Sci. Rep,
doi:10.1038/s41598-020-76488-2Siow, Lee, Zhang, Saffari, Ng, Encephalitis as a neurological complication of COVID-19: A systematic review and meta-analysis of incidence, outcomes, and predictors, Eur. J. Neurol,
doi:10.1111/ene.14913Spinato, Fabbris, Polesel, Cazzador, Borsetto et al., Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection, JAMA Neurol,
doi:10.1001/jama.2020.6771Stoian, Stoian, Bajko, Maier, Andone et al., Autoimmune Encephalitis in COVID-19 Infection: Our Experience and Systematic Review of the Literature, Biomedicines,
doi:10.3390/biomedicines10040774Tabassum, Iqbal, Sultan, Alhuthali, Alshubaili et al., Dysregulated Bradykinin: Mystery in the Pathogenesis of COVID-19, Mediat. Inflamm,
doi:10.1155/2022/7423537Tabor-Godwin, Ruller, Bagalso, An, Pagarigan et al., A novel population of myeloid cells responding to coxsackievirus infection assists in the dissemination of virus within the neonatal CNS, J. Neurosci. Off. J. Soc. Neurosci,
doi:10.1523/JNEUROSCI.1860-10.2010Tavassoly, Safavi, Tavassoly, Seeding Brain Protein Aggregation by SARS-CoV-2 as a Possible Long-Term Complication of COVID-19 Infection, ACS Chem. Neurosci,
doi:10.1021/acschemneuro.0c00676Tong, Wong, Zhu, Fastenberg, Tham, The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis, Otolaryngol. Head. Neck Surg. Off. J. Am. Acad. Otolaryngol. Head Neck Surg,
doi:10.1177/0194599820926473Toscano, Palmerini, Ravaglia, Ruiz, Invernizzi et al., Guillain-Barré Syndrome Associated with SARS-CoV-2, N. Engl. J. Med,
doi:10.1056/NEJMc2009191Trejo-Gabriel-Galán, Stroke as a complication and prognostic factor of COVID-19. Ictus como complicación y como factor pronóstico de COVID-19, Neurologia,
doi:10.1016/j.nrl.2020.04.015Troccoli, Tratamiento trombolítico del ictus isquémico agudo, Gac. Méd
Troyer, Kohn, Hong, Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms, Brain Behav. Immun,
doi:10.1016/j.bbi.2020.04.027Tsai, Hsieh, Chang, Neurological manifestations in severe acute respiratory syndrome, Acta Neurol. Taiwanica
Tsuruoka, Wakaumi, Ioka, Yamamoto, Ando et al., Angiotensin II receptor blocker-induces blunted taste sensitivity: Comparison of candesartan and valsartan, Br. J. Clin. Pharmacol,
doi:10.1111/j.1365-2125.2005.02394.xUygun, Ertaş, Ekizo Glu, Bolay, Özge et al., Headache characteristics in COVID-19 pandemic-a survey study, J. Headache Pain,
doi:10.1186/s10194-020-01188-1Vaira, Deiana, Fois, Pirina, Madeddu et al., Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases, Head Neck,
doi:10.1002/hed.26204Vaira, Salzano, Fois, Piombino, De Riu, Potential pathogenesis of ageusia and anosmia in COVID-19 patients, Int. Forum Allergy Rhinol,
doi:10.1002/alr.22593Van Riel, Verdijk, Kuiken, The olfactory nerve: A shortcut for influenza and other viral diseases into the central nervous system, J. Pathol,
doi:10.1002/path.4461Varatharaj, Thomas, Ellul, Davies, Pollak et al., Neurological and neuropsychiatric complications of COVID-19 in 153 patients: A UK-wide surveillance study, Lancet Psychiatry,
doi:10.1016/S2215-0366(20)30287-XVerma, Lo, Chapagain, Lum, Kumar et al., West Nile virus infection modulates human brain microvascular endothelial cells tight junction proteins and cell adhesion molecules: Transmigration across the in vitro blood-brain barrier, Virology,
doi:10.1016/j.virol.2008.11.047Wang, Kream, Stefano, Long-Term Respiratory and Neurological Sequelae of COVID-19, Med. Sci. Monit. Int. Med. J. Exp. Clin. Res,
doi:10.12659/MSM.928996Wang, Liu, Liu, Li, Lin et al., SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19, J. Hepatol,
doi:10.1016/j.jhep.2020.05.002Wei, Wang, Niu, Ye, Peng et al., Diarrhea Is Associated With Prolonged Symptoms and Viral Carriage in Corona Virus Disease, Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc,
doi:10.1016/j.cgh.2020.04.030Wright, Alex, Nguyen, Bader, Gurakar et al., Multiplex cytokine profiling of initial therapeutic response in patients with chronic hepatitis C virus infection, Dig. Dis. Sci,
doi:10.1007/s10620-005-2940-yXu, Zhong, Deng, Peng, Dan et al., High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, Int. J. Oral Sci,
doi:10.1038/s41368-020-0074-xYang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study, Lancet Respir. Med,
doi:10.1016/S2213-2600(20)30079-5Yeh, Collins, Cohen, Duffner, Faden, Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis, Pediatrics
Yiannopoulou, Vakrakou, Anastasiou, Sourdi, Tzartos et al., Cerebrospinal Fluid Anti-Neuronal Autoantibodies in COVID-19-Associated Limbic Encephalitis with Acute Cerebellar Ataxia and Myoclonus Syndrome: Case Report and Literature Review, Diagnostics,
doi:10.3390/diagnostics13122055Ying, Qian, Kun, Drugs supply and pharmaceutical care management practices at a designated hospital during the COVID-19 epidemic, Res. Soc. Adm. Pharm. RSAP,
doi:10.1016/j.sapharm.2020.04.001Zhang, He, Yao, Tang, Ma et al., COVID-19-associated monocytic encephalitis (CAME): Histological and proteomic evidence from autopsy, Signal Transduct. Target. Ther,
doi:10.1038/s41392-022-01291-6Zhao, Shen, Zhou, Liu, Chen, Guillain-Barré syndrome associated with SARS-CoV-2 infection: Causality or coincidence?, Lancet Neurol,
doi:10.1016/S1474-4422(20)30109-5Zou, Chen, Zou, Han, Hao et al., Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection, Front. Med,
doi:10.1007/s11684-020-0754-0DOI record:
{
"DOI": "10.3390/biomedicines12061147",
"ISSN": [
"2227-9059"
],
"URL": "http://dx.doi.org/10.3390/biomedicines12061147",
"abstract": "<jats:p>The SARS-CoV-2 virus has spread rapidly despite implementing strategies to reduce its transmission. The disease caused by this virus has been associated with a diverse range of symptoms, including common neurological manifestations such as dysgeusia, anosmia, and myalgias. Additionally, numerous cases of severe neurological complications associated with this disease have been reported, including encephalitis, stroke, seizures, and Guillain–Barré syndrome, among others. Given the high prevalence of neurological manifestations in this disease, the objective of this review is to analyze the mechanisms by which this virus can affect the nervous system, from its direct invasion to aberrant activation of the immune system and other mechanisms involved in the symptoms, including neuropsychiatric manifestations, to gain a better understanding of the disease and thus facilitate the search for effective therapeutic strategies.</jats:p>",
"alternative-id": [
"biomedicines12061147"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0123-3629",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Ariza",
"given": "Daniela",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla 080001, Colombia"
}
],
"family": "Castellar-Visbal",
"given": "Lily",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6203-181X",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Marquina",
"given": "Maria",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2169-3208",
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias Jurídicas y Sociales, Centro de Investigación en Estudios Fronterizos, Cúcuta 540001, Colombia"
}
],
"authenticated-orcid": false,
"family": "Rivera-Porras",
"given": "Diego",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0765-2290",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Galbán",
"given": "Nestor",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0761-5879",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Santeliz",
"given": "Raquel",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1878-3432",
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla 080001, Colombia"
}
],
"authenticated-orcid": false,
"family": "Gutiérrez-Rey",
"given": "Melissa",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6604-4212",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Parra",
"given": "Heliana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla 080001, Colombia"
}
],
"family": "Vargas-Manotas",
"given": "José",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"family": "Torres",
"given": "Wheeler",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0009-0003-3729-8066",
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla 080001, Colombia"
}
],
"authenticated-orcid": false,
"family": "Quintana-Espinosa",
"given": "Laura",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6652-8834",
"affiliation": [
{
"name": "Endocrine and Metabolic Diseases Research Center, School of Medicine, Universidad del Zulia, Maracaibo 4002, Venezuela"
}
],
"authenticated-orcid": false,
"family": "Manzano",
"given": "Alexander",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3120-4757",
"affiliation": [
{
"name": "Departamento de Ciencias Sociales, Universidad de la Costa, Barranquilla 080001, Colombia"
}
],
"authenticated-orcid": false,
"family": "Cudris-Torres",
"given": "Lorena",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1880-8887",
"affiliation": [
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Barranquilla 080001, Colombia"
},
{
"name": "Universidad Simón Bolívar, Facultad de Ciencias de la Salud, Centro de Investigaciones en Ciencias de la Vida, Barranquilla 080001, Colombia"
}
],
"authenticated-orcid": false,
"family": "Bermúdez",
"given": "Valmore",
"sequence": "additional"
}
],
"container-title": "Biomedicines",
"container-title-short": "Biomedicines",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
5,
22
]
],
"date-time": "2024-05-22T14:00:11Z",
"timestamp": 1716386411000
},
"deposited": {
"date-parts": [
[
2024,
5,
22
]
],
"date-time": "2024-05-22T15:20:49Z",
"timestamp": 1716391249000
},
"funder": [
{
"name": "Universidad Simón Bolívar, Vicerrectoría de Investigación, Extensión e Innovación, Barranquilla, Colombia"
}
],
"indexed": {
"date-parts": [
[
2024,
5,
23
]
],
"date-time": "2024-05-23T00:27:28Z",
"timestamp": 1716424048476
},
"is-referenced-by-count": 0,
"issue": "6",
"issued": {
"date-parts": [
[
2024,
5,
22
]
]
},
"journal-issue": {
"issue": "6",
"published-online": {
"date-parts": [
[
2024,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
5,
22
]
],
"date-time": "2024-05-22T00:00:00Z",
"timestamp": 1716336000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2227-9059/12/6/1147/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1147",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
5,
22
]
]
},
"published-online": {
"date-parts": [
[
2024,
5,
22
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"key": "ref_1",
"unstructured": "World Health Organization (2024). COVID-19 Deaths|WHO COVID-19, World Health Organization."
},
{
"DOI": "10.3389/fimmu.2023.1117464",
"article-title": "Long COVID: A review and proposed visualization of the complexity of long COVID",
"author": "Perumal",
"doi-asserted-by": "crossref",
"first-page": "1117464",
"journal-title": "Front. Immunol.",
"key": "ref_2",
"volume": "14",
"year": "2023"
},
{
"article-title": "Long COVID: Major findings, mechanisms and recommendations. Nature reviews",
"author": "Davis",
"first-page": "133",
"journal-title": "Microbiology",
"key": "ref_3",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.3389/fmed.2022.1017257",
"article-title": "Post-COVID-19 syndrome symptoms after mild and moderate SARS-CoV-2 infection",
"author": "Nusir",
"doi-asserted-by": "crossref",
"first-page": "1017257",
"journal-title": "Front. Med.",
"key": "ref_4",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.1080/07853890.2022.2076901",
"article-title": "Pathophysiology and mechanism of long COVID: A comprehensive review",
"author": "Chalon",
"doi-asserted-by": "crossref",
"first-page": "1473",
"journal-title": "Ann. Med.",
"key": "ref_5",
"volume": "54",
"year": "2022"
},
{
"DOI": "10.1016/j.tmaid.2023.102606",
"article-title": "The global challenges of the long COVID-19 in adults and children",
"doi-asserted-by": "crossref",
"first-page": "102606",
"journal-title": "Travel. Med. Infect. Dis.",
"key": "ref_6",
"volume": "54",
"year": "2023"
},
{
"DOI": "10.1038/s41564-020-0695-z",
"article-title": "The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2",
"author": "Gorbalenya",
"doi-asserted-by": "crossref",
"first-page": "536",
"journal-title": "Nat. Microbiol.",
"key": "ref_7",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.24171/j.phrp.2020.11.1.02",
"article-title": "Identification of Coronavirus Isolated from a Patient in Korea with COVID-19",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Osong Public Health Res. Perspect.",
"key": "ref_8",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1007/s11684-020-0754-0",
"article-title": "Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection",
"author": "Zou",
"doi-asserted-by": "crossref",
"first-page": "185",
"journal-title": "Front. Med.",
"key": "ref_9",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/path.1570",
"article-title": "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis",
"author": "Hamming",
"doi-asserted-by": "crossref",
"first-page": "631",
"journal-title": "J. Pathol.",
"key": "ref_10",
"volume": "203",
"year": "2004"
},
{
"DOI": "10.1007/s00134-020-06062-x",
"article-title": "High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study",
"author": "Helms",
"doi-asserted-by": "crossref",
"first-page": "1089",
"journal-title": "Intensive Care Med.",
"key": "ref_11",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1093/eurheartj/ehaa288",
"article-title": "COVID-19-related myocarditis in a 21-year-old female patient",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "1859",
"journal-title": "Eur. Heart J.",
"key": "ref_12",
"volume": "41",
"year": "2020"
},
{
"article-title": "Diarrhea Is Associated With Prolonged Symptoms and Viral Carriage in Corona Virus Disease 2019",
"author": "Wei",
"first-page": "1753",
"journal-title": "Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc.",
"key": "ref_13",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.ekir.2020.05.005",
"article-title": "Kidney Biopsy Findings in a Critically Ill COVID-19 Patient with Dialysis-Dependent Acute Kidney Injury: A Case against \"SARS-CoV-2 Nephropathy",
"author": "Rossi",
"doi-asserted-by": "crossref",
"first-page": "1100",
"journal-title": "Kidney Int. Rep.",
"key": "ref_14",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1016/j.jhep.2020.05.002",
"article-title": "SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "807",
"journal-title": "J. Hepatol.",
"key": "ref_15",
"volume": "74",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00524-2020",
"article-title": "Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study",
"author": "Wen",
"doi-asserted-by": "crossref",
"first-page": "2000524",
"journal-title": "Eur. Respir. J.",
"key": "ref_16",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1101/2020.04.08.20057794",
"doi-asserted-by": "crossref",
"key": "ref_17",
"unstructured": "Petrilli, C.M., Jones, S.A., Yang, J., Rajagopalan, H., O’Donnell, L., Chernyak, Y., and Horwitz, L.I. (2020). Factors associated with hospitalization and critical illness among 4103 patients with COVID-19 disease in New York City. MedRxiv."
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref_18",
"volume": "395",
"year": "2020"
},
{
"article-title": "Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection",
"author": "Spinato",
"first-page": "2089",
"journal-title": "JAMA Neurol.",
"key": "ref_19",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/s00405-020-05965-1",
"article-title": "Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study",
"author": "Lechien",
"doi-asserted-by": "crossref",
"first-page": "2251",
"journal-title": "Eur. Arch. Oto-Rhino-Laryngol.",
"key": "ref_20",
"volume": "277",
"year": "2020"
},
{
"DOI": "10.1007/s13365-020-00840-5",
"article-title": "COVID-19 and the nervous system",
"author": "Berger",
"doi-asserted-by": "crossref",
"first-page": "143",
"journal-title": "J. Neurovirol.",
"key": "ref_21",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"article-title": "Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China",
"author": "Mao",
"doi-asserted-by": "crossref",
"first-page": "683",
"journal-title": "JAMA Neurol.",
"key": "ref_22",
"volume": "77",
"year": "2020"
},
{
"article-title": "Rhabdomyolysis in COVID-19 Patients: A Retrospective Observational Study",
"author": "Haroun",
"first-page": "e12552",
"journal-title": "Cureus",
"key": "ref_23",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(20)30287-X",
"article-title": "Neurological and neuropsychiatric complications of COVID-19 in 153 patients: A UK-wide surveillance study",
"author": "Varatharaj",
"doi-asserted-by": "crossref",
"first-page": "875",
"journal-title": "Lancet Psychiatry",
"key": "ref_24",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.amsu.2022.103440",
"article-title": "Post COVID-19 neurological complications; a meta-analysis",
"author": "Ahmed",
"doi-asserted-by": "crossref",
"first-page": "103440",
"journal-title": "Ann. Med. Surg.",
"key": "ref_25",
"volume": "76",
"year": "2022"
},
{
"article-title": "Long-Term Respiratory and Neurological Sequelae of COVID-19",
"author": "Wang",
"first-page": "e928996",
"journal-title": "Med. Sci. Monit. Int. Med. J. Exp. Clin. Res.",
"key": "ref_26",
"volume": "26",
"year": "2020"
},
{
"article-title": "COVID-19 Related Acute Hemorrhagic Necrotizing Encephalitis: A Report of Two Cases and Literature Review",
"author": "Mullaguri",
"first-page": "e14236",
"journal-title": "Cureus",
"key": "ref_27",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.semerg.2020.05.004",
"article-title": "Neurological manifestations of SARS-CoV-2 infection",
"doi-asserted-by": "crossref",
"first-page": "106",
"journal-title": "Semergen",
"key": "ref_28",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1007/s00401-020-02166-2",
"article-title": "Neuropathology of COVID-19: A spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology",
"author": "Reichard",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Acta Neuropathol.",
"key": "ref_29",
"volume": "140",
"year": "2020"
},
{
"DOI": "10.1007/s00401-020-02190-2",
"article-title": "Microvascular injury and hypoxic damage: Emerging neuropathological signatures in COVID-19",
"author": "Jaunmuktane",
"doi-asserted-by": "crossref",
"first-page": "397",
"journal-title": "Acta Neuropathol.",
"key": "ref_30",
"volume": "140",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31282-4",
"article-title": "Early evidence of pronounced brain involvement in fatal COVID-19 outcomes",
"author": "Kaufmann",
"doi-asserted-by": "crossref",
"first-page": "e109",
"journal-title": "Lancet",
"key": "ref_31",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1212/WNL.0000000000010116",
"article-title": "Early postmortem brain MRI findings in COVID-19 non-survivors",
"author": "Coolen",
"doi-asserted-by": "crossref",
"first-page": "e2016",
"journal-title": "Neurology",
"key": "ref_32",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1212/WNL.0000000000010111",
"article-title": "Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19",
"author": "Kanberg",
"doi-asserted-by": "crossref",
"first-page": "e1754",
"journal-title": "Neurology",
"key": "ref_33",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.3389/fneur.2020.00518",
"article-title": "Neurological manifestations of COVID-19 (SARS-CoV-2): A review",
"author": "Ahmed",
"doi-asserted-by": "crossref",
"first-page": "518",
"journal-title": "Front. Neurol.",
"key": "ref_34",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3390/v12010014",
"doi-asserted-by": "crossref",
"key": "ref_35",
"unstructured": "Desforges, M., Le Coupanec, A., Dubeau, P., Bourgouin, A., Lajoie, L., Dubé, M., and Talbot, P.J. (2019). Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System?. Viruses, 12."
},
{
"DOI": "10.1542/peds.113.1.e73",
"article-title": "Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis",
"author": "Yeh",
"doi-asserted-by": "crossref",
"first-page": "e73",
"journal-title": "Pediatrics",
"key": "ref_36",
"volume": "113",
"year": "2004"
},
{
"DOI": "10.1128/JVI.00404-18",
"article-title": "Axonal Transport Enables Neuron-to-Neuron Propagation of Human Coronavirus OC43",
"author": "Wong",
"doi-asserted-by": "crossref",
"first-page": "e00404-18",
"journal-title": "J. Virol.",
"key": "ref_37",
"volume": "92",
"year": "2018"
},
{
"DOI": "10.1093/infdis/jit123",
"article-title": "Differential cell line susceptibility to the emerging novel human betacoronavirus 2c EMC/2012: Implications for disease pathogenesis and clinical manifestation",
"author": "Chan",
"doi-asserted-by": "crossref",
"first-page": "1743",
"journal-title": "J. Infect. Dis.",
"key": "ref_38",
"volume": "207",
"year": "2013"
},
{
"DOI": "10.14573/altex.1609122",
"article-title": "A human brain microphysiological system derived from induced pluripotent stem cells to study neurological diseases and toxicity",
"author": "Pamies",
"doi-asserted-by": "crossref",
"first-page": "362",
"journal-title": "ALTEX",
"key": "ref_39",
"volume": "34",
"year": "2017"
},
{
"article-title": "Infectability of human BrainSphere neurons suggests neurotropism of SARS-CoV-2",
"author": "Bullen",
"first-page": "665",
"journal-title": "ALTEX",
"key": "ref_40",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1371/journal.pbio.3001845",
"doi-asserted-by": "crossref",
"key": "ref_41",
"unstructured": "Mesci, P., de Souza, J.S., Martin-Sancho, L., Macia, A., Saleh, A., Yin, X., Snethlage, C., Adams, J.W., Avansini, S.H., and Herai, R.H. (2022). SARS-CoV-2 infects human brain organoids causing cell death and loss of synapses that can be rescued by treatment with Sofosbuvir. PLoS Biol., 20."
},
{
"DOI": "10.1038/s41392-022-01241-2",
"article-title": "Enhanced replication of SARS-CoV-2 Omicron BA.2 in human forebrain and midbrain organoids",
"author": "Hou",
"doi-asserted-by": "crossref",
"first-page": "381",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_42",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1056/NEJMc2011400",
"article-title": "Multiorgan and Renal Tropism of SARS-CoV-2",
"author": "Puelles",
"doi-asserted-by": "crossref",
"first-page": "590",
"journal-title": "N. Engl. J. Med.",
"key": "ref_43",
"volume": "383",
"year": "2020"
},
{
"article-title": "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2",
"author": "Moriguchi",
"first-page": "55",
"journal-title": "Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis.",
"key": "ref_44",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.3390/ijerph18010284",
"doi-asserted-by": "crossref",
"key": "ref_45",
"unstructured": "Qi, J., Zhou, Y., Hua, J., Zhang, L., Bian, J., Liu, B., Zhao, Z., and Jin, S. (2021). The scRNA-seq Expression Profiling of the Receptor ACE2 and the Cellular Protease TMPRSS2 Reveals Human Organs Susceptible to SARS-CoV-2 Infection. Int. J. Environ. Res. Public Health, 18."
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "ref_46",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1128/JVI.02029-09",
"article-title": "Retrograde axon transport of herpes simplex virus and pseudorabies virus: A live-cell comparative analysis",
"author": "Antinone",
"doi-asserted-by": "crossref",
"first-page": "1504",
"journal-title": "J. Virol.",
"key": "ref_47",
"volume": "84",
"year": "2010"
},
{
"DOI": "10.1371/journal.ppat.1007188",
"doi-asserted-by": "crossref",
"key": "ref_48",
"unstructured": "MacGibeny, M.A., Koyuncu, O.O., Wirblich, C., Schnell, M.J., and Enquist, L.W. (2018). Retrograde axonal transport of rabies virus is unaffected by interferon treatment but blocked by emetine locally in axons. PLoS Pathog., 14."
},
{
"DOI": "10.1002/path.4461",
"article-title": "The olfactory nerve: A shortcut for influenza and other viral diseases into the central nervous system",
"author": "Verdijk",
"doi-asserted-by": "crossref",
"first-page": "277",
"journal-title": "J. Pathol.",
"key": "ref_49",
"volume": "235",
"year": "2015"
},
{
"DOI": "10.1001/jamaneurol.2020.2125",
"article-title": "Magnetic Resonance Imaging Alteration of the Brain in a Patient With Coronavirus Disease 2019 (COVID-19) and Anosmia",
"author": "Politi",
"doi-asserted-by": "crossref",
"first-page": "1028",
"journal-title": "JAMA Neurol.",
"key": "ref_50",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1038/s41593-020-00758-5",
"article-title": "Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19",
"author": "Meinhardt",
"doi-asserted-by": "crossref",
"first-page": "168",
"journal-title": "Nat. Neurosci.",
"key": "ref_51",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1126/sciadv.abc5801",
"article-title": "Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia",
"author": "Brann",
"doi-asserted-by": "crossref",
"first-page": "eabc5801",
"journal-title": "Sci. Adv.",
"key": "ref_52",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.08.139329",
"doi-asserted-by": "crossref",
"key": "ref_53",
"unstructured": "Nampoothiri, S., Sauve, F., Ternier, G., Fernandois, D., Coelho, C., Imbernon, M., and Prevot, V. (2020). The hypothalamus as a hub for putative SARS-CoV-2 brain infection. BioRxiv."
},
{
"DOI": "10.1186/s12974-023-02861-3",
"article-title": "Differential effects of SARS-CoV-2 variants on central nervous system cells and blood-brain barrier functions",
"author": "Proust",
"doi-asserted-by": "crossref",
"first-page": "184",
"journal-title": "J. Neuroinflamm.",
"key": "ref_54",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.3389/fmolb.2021.690655",
"doi-asserted-by": "crossref",
"key": "ref_55",
"unstructured": "Milanetti, E., Miotto, M., Di Rienzo, L., Nagaraj, M., Monti, M., Golbek, T.W., Gosti, G., Roeters, S.J., Weidner, T., and Otzen, D.E. (2021). In-Silico Evidence for a Two Receptor Based Strategy of SARS-CoV-2. Front. Mol. Biosci., 8."
},
{
"DOI": "10.1016/j.antiviral.2020.104759",
"article-title": "A potential role for integrins in host cell entry by SARS-CoV-2",
"author": "Sigrist",
"doi-asserted-by": "crossref",
"first-page": "104759",
"journal-title": "Antivir. Res.",
"key": "ref_56",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.1016/j.virol.2008.11.047",
"article-title": "West Nile virus infection modulates human brain microvascular endothelial cells tight junction proteins and cell adhesion molecules: Transmigration across the in vitro blood-brain barrier",
"author": "Verma",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "Virology",
"key": "ref_57",
"volume": "385",
"year": "2009"
},
{
"DOI": "10.1523/JNEUROSCI.1860-10.2010",
"article-title": "A novel population of myeloid cells responding to coxsackievirus infection assists in the dissemination of virus within the neonatal CNS",
"author": "Ruller",
"doi-asserted-by": "crossref",
"first-page": "8676",
"journal-title": "J. Neurosci. Off. J. Soc. Neurosci.",
"key": "ref_58",
"volume": "30",
"year": "2010"
},
{
"DOI": "10.1002/jmv.25915",
"article-title": "Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)",
"author": "Bryce",
"doi-asserted-by": "crossref",
"first-page": "699",
"journal-title": "J. Med. Virol.",
"key": "ref_59",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2022.1070379",
"article-title": "Markers of blood-brain barrier disruption increase early and persistently in COVID-19 patients with neurological manifestations",
"author": "Bonetto",
"doi-asserted-by": "crossref",
"first-page": "1070379",
"journal-title": "Front. Immunol.",
"key": "ref_60",
"volume": "13",
"year": "2022"
},
{
"article-title": "Immune Dysregulation during and after COVID-19: “Tomorrow Never Dies” Situation",
"author": "Patil",
"first-page": "e00024",
"journal-title": "J. Transl. Crit. Care Med.",
"key": "ref_61",
"volume": "5",
"year": "1793"
},
{
"DOI": "10.1007/s10620-005-2940-y",
"article-title": "Multiplex cytokine profiling of initial therapeutic response in patients with chronic hepatitis C virus infection",
"author": "Wright",
"doi-asserted-by": "crossref",
"first-page": "1793",
"journal-title": "Dig. Dis. Sci.",
"key": "ref_62",
"volume": "50",
"year": "2005"
},
{
"DOI": "10.1007/s00134-020-05991-x",
"article-title": "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China",
"author": "Ruan",
"doi-asserted-by": "crossref",
"first-page": "846",
"journal-title": "Intensive Care Med.",
"key": "ref_63",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2021.06.002",
"article-title": "COVID-19: Activation, pathogenesis and therapeutic strategies",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "2",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "ref_64",
"volume": "61",
"year": "2021"
},
{
"DOI": "10.3389/fncel.2015.00028",
"article-title": "Systemic inflammation and the brain: Novel roles of genetic, molecular, and environmental cues as drivers of neurodegeneration",
"author": "Sankowski",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Front. Cell. Neurosci.",
"key": "ref_65",
"volume": "9",
"year": "2015"
},
{
"DOI": "10.1212/NXI.0000000000000781",
"article-title": "Guillain-Barré syndrome: The first documented COVID-19-triggered autoimmune neurologic disease: More to come with myositis in the offing",
"author": "Dalakas",
"doi-asserted-by": "crossref",
"first-page": "e781",
"journal-title": "Neurol. Neuroimmunol. Neuroinflamm.",
"key": "ref_66",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.bbadis.2014.06.013",
"article-title": "Pathogenesis of immune-mediated neuropathies",
"author": "Dalakas",
"doi-asserted-by": "crossref",
"first-page": "658",
"journal-title": "Biochim. Biophys. Acta",
"key": "ref_67",
"volume": "185",
"year": "2015"
},
{
"DOI": "10.1016/j.pediatrneurol.2020.10.002",
"article-title": "N-Methyl-d-Aspartate Receptor Encephalitis Associated with COVID-19 Infection in a Toddler",
"author": "Burr",
"doi-asserted-by": "crossref",
"first-page": "75",
"journal-title": "Pediatr. Neurol.",
"key": "ref_68",
"volume": "114",
"year": "2021"
},
{
"DOI": "10.1186/s12883-021-02449-5",
"doi-asserted-by": "crossref",
"key": "ref_69",
"unstructured": "Durovic, E., Bien, C., Bien, C.G., and Isenmann, S. (2021). MOG antibody-associated encephalitis secondary to COVID-19: Case report. BMC Neurol., 21."
},
{
"DOI": "10.3390/diagnostics13122055",
"doi-asserted-by": "crossref",
"key": "ref_70",
"unstructured": "Yiannopoulou, K., Vakrakou, A.G., Anastasiou, A., Sourdi, N.G.A., Tzartos, J.S., Kilidireas, C., and Dimitrakopoulos, A. (2023). Cerebrospinal Fluid Anti-Neuronal Autoantibodies in COVID-19-Associated Limbic Encephalitis with Acute Cerebellar Ataxia and Myoclonus Syndrome: Case Report and Literature Review. Diagnostics, 13."
},
{
"DOI": "10.3389/fneur.2021.764197",
"article-title": "Acute Psychosis Due to Anti-N-Methyl D-Aspartate Receptor Encephalitis Following COVID-19 Vaccination: A Case Report",
"author": "Flannery",
"doi-asserted-by": "crossref",
"first-page": "764197",
"journal-title": "Front. Neurol.",
"key": "ref_71",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3390/vaccines11030576",
"doi-asserted-by": "crossref",
"key": "ref_72",
"unstructured": "Abdelhady, M., Husain, M.A., Hawas, Y., Elazb, M.A., Mansour, L.S., Mohamed, M., Abdelwahab, M.M., Aljabali, A., and Negida, A. (2023). Encephalitis following COVID-19 Vaccination: A Systematic Review. Vaccines, 11."
},
{
"DOI": "10.1016/j.jneuroim.2021.577739",
"article-title": "Longitudinally extensive transverse myelitis with anti-myelin oligodendrocyte glycoprotein antibodies following SARS-CoV-2 infection",
"author": "Rato",
"doi-asserted-by": "crossref",
"first-page": "577739",
"journal-title": "J. Neuroimmunol.",
"key": "ref_73",
"volume": "361",
"year": "2021"
},
{
"DOI": "10.3390/biomedicines10040774",
"doi-asserted-by": "crossref",
"key": "ref_74",
"unstructured": "Stoian, A., Stoian, M., Bajko, Z., Maier, S., Andone, S., Cioflinc, R.A., Motataianu, A., Barcutean, L., and Balasa, R. (2022). Autoimmune Encephalitis in COVID-19 Infection: Our Experience and Systematic Review of the Literature. Biomedicines, 10."
},
{
"DOI": "10.3390/cells12050816",
"doi-asserted-by": "crossref",
"key": "ref_75",
"unstructured": "Leng, A., Shah, M., Ahmad, S.A., Premraj, L.W.K., Bassi, G.L., Pardo, C.A., Choi, A., and Cho, S.M. (2023). Pathogenesis Underlying Neurological Manifestations of Long COVID Syndrome and Potential Therapeutics. Cells, 12."
},
{
"article-title": "A hypothesized role for dysregulated bradykinin signaling in COVID-19 respiratory complications",
"author": "Roche",
"first-page": "7265",
"journal-title": "FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol.",
"key": "ref_76",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.vph.2020.106826",
"article-title": "A new storm on the horizon in COVID-19: Bradykinin-induced vascular complications",
"author": "McCarthy",
"doi-asserted-by": "crossref",
"first-page": "106826",
"journal-title": "Vasc. Pharmacol.",
"key": "ref_77",
"volume": "137",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-76488-2",
"article-title": "SARS-CoV-2 receptor is co-expressed with elements of the kinin-kallikrein, renin-angiotensin and coagulation systems in alveolar cell",
"author": "Jara",
"doi-asserted-by": "crossref",
"first-page": "19522",
"journal-title": "Sci. Rep.",
"key": "ref_78",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1155/2022/7423537",
"article-title": "Dysregulated Bradykinin: Mystery in the Pathogenesis of COVID-19",
"author": "Tabassum",
"doi-asserted-by": "crossref",
"first-page": "7423537",
"journal-title": "Mediat. Inflamm.",
"key": "ref_79",
"volume": "2022",
"year": "2022"
},
{
"DOI": "10.1177/0194599820926473",
"article-title": "The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis",
"author": "Tong",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Otolaryngol. Head. Neck Surg. Off. J. Am. Acad. Otolaryngol. Head Neck Surg.",
"key": "ref_80",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2008597",
"article-title": "Neurologic Features in Severe SARS-CoV-2 Infection",
"author": "Helms",
"doi-asserted-by": "crossref",
"first-page": "2268",
"journal-title": "N. Engl. J. Med.",
"key": "ref_81",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Lancet Respir. Med.",
"key": "ref_82",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1002/ana.25783",
"article-title": "Steroid-Responsive Encephalitis in Coronavirus Disease 2019",
"author": "Pilotto",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Ann. Neurol.",
"key": "ref_83",
"volume": "88",
"year": "2020"
},
{
"DOI": "10.1136/jnnp-2020-323586",
"article-title": "Characteristics of ischaemic stroke associated with COVID-19",
"author": "Beyrouti",
"doi-asserted-by": "crossref",
"first-page": "889",
"journal-title": "J. Neurol. Neurosurg. Psychiatry",
"key": "ref_84",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.5812/ircmj.102828",
"article-title": "Frequent Convulsive Seizures in an Adult Patient with COVID-19: A Case Report",
"author": "Karimi",
"doi-asserted-by": "crossref",
"first-page": "e102828",
"journal-title": "Iran. Red. Crescent Med. J.",
"key": "ref_85",
"volume": "22",
"year": "2020"
},
{
"article-title": "Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2",
"author": "Beato",
"first-page": "230",
"journal-title": "J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas.",
"key": "ref_86",
"volume": "77",
"year": "2020"
},
{
"DOI": "10.1007/s15010-015-0720-y",
"article-title": "Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV)",
"author": "Arabi",
"doi-asserted-by": "crossref",
"first-page": "495",
"journal-title": "Infection",
"key": "ref_87",
"volume": "43",
"year": "2015"
},
{
"DOI": "10.1159/000453066",
"article-title": "Coronavirus Infections in the Central Nervous System and Respiratory Tract Show Distinct Features in Hospitalized Children",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "163",
"journal-title": "Intervirology",
"key": "ref_88",
"volume": "59",
"year": "2016"
},
{
"DOI": "10.1111/ene.14913",
"article-title": "Encephalitis as a neurological complication of COVID-19: A systematic review and meta-analysis of incidence, outcomes, and predictors",
"author": "Siow",
"doi-asserted-by": "crossref",
"first-page": "3491",
"journal-title": "Eur. J. Neurol.",
"key": "ref_89",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1038/s41392-022-01291-6",
"article-title": "COVID-19-associated monocytic encephalitis (CAME): Histological and proteomic evidence from autopsy",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_90",
"volume": "8",
"year": "2023"
},
{
"article-title": "COVID-19 vaccines and neurological complications: A systematic review. Zeitschrift fur Naturforschung",
"author": "Allahyari",
"first-page": "1",
"journal-title": "J. Biosci.",
"key": "ref_91",
"volume": "78",
"year": "2022"
},
{
"DOI": "10.1016/j.tmaid.2020.101642",
"article-title": "Sars-Cov-2: Underestimated damage to nervous system",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "101642",
"journal-title": "Travel Med. Infect. Dis.",
"key": "ref_92",
"volume": "36",
"year": "2020"
},
{
"article-title": "Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection",
"author": "Pizzarotti",
"first-page": "e43",
"journal-title": "Eur. J. Neurol.",
"key": "ref_93",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1148/radiol.2020201187",
"article-title": "COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: Imaging Features",
"author": "Poyiadji",
"doi-asserted-by": "crossref",
"first-page": "E119",
"journal-title": "Radiology",
"key": "ref_94",
"volume": "296",
"year": "2020"
},
{
"DOI": "10.1177/19418744211055360",
"article-title": "COVID-19-Associated Acute Asymmetric Hemorrhagic Necrotizing Encephalopathy: A Case Report",
"author": "Jomaa",
"doi-asserted-by": "crossref",
"first-page": "371",
"journal-title": "Neurohospitalist",
"key": "ref_95",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.4103/aian.aian_528_21",
"article-title": "Acute Hemorrhagic Necrotizing Encephalopathy in Patients with COVID-19",
"author": "Nandan",
"doi-asserted-by": "crossref",
"first-page": "511",
"journal-title": "Ann. Indian Acad. Neurol.",
"key": "ref_96",
"volume": "25",
"year": "2022"
},
{
"DOI": "10.1212/NXI.0000000000000789",
"article-title": "COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia",
"author": "Dixon",
"doi-asserted-by": "crossref",
"first-page": "e789",
"journal-title": "Neurol. Neuroimmunol. Neuroinflamm.",
"key": "ref_97",
"volume": "7",
"year": "2020"
},
{
"article-title": "Acute Necrotizing Encephalopathy Associated with SARS-CoV-2 Exposure in a Pediatric Patient",
"author": "Romero",
"first-page": "e15018",
"journal-title": "Cureus",
"key": "ref_98",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1177/1756286420985175",
"article-title": "Extensive cerebellar involvement and cognitive impairment in COVID-19-associated acute necrotizing encephalopathy",
"author": "Ciolac",
"doi-asserted-by": "crossref",
"first-page": "1756286420985175",
"journal-title": "Ther. Adv. Neurol. Disord.",
"key": "ref_99",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1136/jnnp-2020-323678",
"article-title": "COVID-19-associated acute necrotising encephalopathy successfully treated with steroids and polyvalent immunoglobulin with unusual IgG targeting the cerebral fibre network",
"author": "Delamarre",
"doi-asserted-by": "crossref",
"first-page": "1004",
"journal-title": "J. Neurol. Neurosurg. Psychiatry",
"key": "ref_100",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1186/s12879-022-07610-0",
"doi-asserted-by": "crossref",
"key": "ref_101",
"unstructured": "Pongpitakmetha, T., Hemachudha, P., Rattanawong, W., Thanapornsangsuth, P., Viswanathan, A., and Hemachudha, T. (2022). COVID-19 related acute necrotizing encephalopathy with extremely high interleukin-6 and RANBP2 mutation in a patient with recently immunized inactivated virus vaccine and no pulmonary involvement. BMC Infect. Dis., 22."
},
{
"DOI": "10.1016/j.thromres.2020.07.047",
"article-title": "D-dimer level is associated with the severity of COVID-19",
"author": "Yu",
"doi-asserted-by": "crossref",
"first-page": "219",
"journal-title": "Thromb. Res.",
"key": "ref_102",
"volume": "195",
"year": "2020"
},
{
"DOI": "10.1007/s00415-021-10837-7",
"article-title": "Ischemic stroke associated with COVID-19: A systematic review and meta-analysis",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "1731",
"journal-title": "J. Neurol.",
"key": "ref_103",
"volume": "269",
"year": "2022"
},
{
"article-title": "Tratamiento trombolítico del ictus isquémico agudo",
"author": "Troccoli",
"first-page": "183",
"journal-title": "Gac. Méd. Caracas",
"key": "ref_104",
"volume": "121",
"year": "2020"
},
{
"DOI": "10.1038/s41577-020-0311-8",
"article-title": "The trinity of COVID-19: Immunity, inflammation and intervention",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "363",
"journal-title": "Nat. Rev. Immunol.",
"key": "ref_105",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1136/svn-2020-000431",
"article-title": "Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "279",
"journal-title": "Stroke Vasc. Neurol.",
"key": "ref_106",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.7754/Clin.Lab.2021.210802",
"doi-asserted-by": "crossref",
"key": "ref_107",
"unstructured": "Medetalibeyoglu, A., Kaytaz, M., Senkal, N., Genc, S., Aktar, I., Omer, B., Oncul, O., and Tukek, T. (2022). Would Tracking Coagulation Together with Inflamation Markers be a Prospect for COVID-19 Disease Prognosis?. Clin. Lab., 68."
},
{
"DOI": "10.1097/WCO.0b013e328012da75",
"article-title": "Why now? Moving from stroke risk factors to stroke triggers",
"author": "Elkind",
"doi-asserted-by": "crossref",
"first-page": "51",
"journal-title": "Curr. Opin. Neurol.",
"key": "ref_108",
"volume": "20",
"year": "2007"
},
{
"DOI": "10.1016/j.jcv.2020.104362",
"article-title": "Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past",
"author": "Giannis",
"doi-asserted-by": "crossref",
"first-page": "104362",
"journal-title": "J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol.",
"key": "ref_109",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1111/jth.14850",
"article-title": "ypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis",
"author": "Panigada",
"doi-asserted-by": "crossref",
"first-page": "1738",
"journal-title": "J. Thromb. Haemost. JTH",
"key": "ref_110",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1007/s12185-020-03029-y",
"article-title": "COVID-19-associated coagulopathy and disseminated intravascular coagulation",
"author": "Asakura",
"doi-asserted-by": "crossref",
"first-page": "45",
"journal-title": "Int. J. Hematol.",
"key": "ref_111",
"volume": "113",
"year": "2021"
},
{
"article-title": "Age-related physiological changes and their clinical significance",
"author": "Boss",
"first-page": "434",
"journal-title": "West. J. Med.",
"key": "ref_112",
"volume": "135",
"year": "1981"
},
{
"DOI": "10.1016/j.nrl.2020.04.015",
"article-title": "Stroke as a complication and prognostic factor of COVID-19. Ictus como complicación y como factor pronóstico de COVID-19",
"doi-asserted-by": "crossref",
"first-page": "318",
"journal-title": "Neurologia",
"key": "ref_113",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1101/cshperspect.a022426",
"article-title": "Seizures and epilepsy: An overview for neuroscientists",
"author": "Stafstrom",
"doi-asserted-by": "crossref",
"first-page": "a022426",
"journal-title": "Cold Spring Harb. Perspect. Med.",
"key": "ref_114",
"volume": "5",
"year": "2015"
},
{
"article-title": "COVID-19-Induced Seizures: A Meta-Analysis of Case Series and Retrospective Cohorts",
"author": "Hussaini",
"first-page": "e28633",
"journal-title": "Cureus",
"key": "ref_115",
"volume": "14",
"year": "2022"
},
{
"article-title": "Estatus epiléptico en niños: Aspectos generales diagnósticos y terapéuticos",
"author": "Diaz",
"first-page": "377",
"journal-title": "Arch. Venez. Farmacol. Ter.",
"key": "ref_116",
"volume": "38",
"year": "2019"
},
{
"DOI": "10.1016/j.lfs.2020.118063",
"article-title": "Update on neurological manifestations of COVID-19",
"doi-asserted-by": "crossref",
"first-page": "118063",
"journal-title": "Life Sci.",
"key": "ref_117",
"volume": "257",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.03.037",
"article-title": "The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19",
"author": "Ye",
"doi-asserted-by": "crossref",
"first-page": "607",
"journal-title": "J. Infect.",
"key": "ref_118",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1111/j.1469-8749.2011.03928.x",
"article-title": "Infectious causes of seizures and epilepsy in the developing world",
"author": "Singhi",
"doi-asserted-by": "crossref",
"first-page": "600",
"journal-title": "Dev. Med. Child Neurol.",
"key": "ref_119",
"volume": "53",
"year": "2011"
},
{
"DOI": "10.1590/0004-282x20190196",
"article-title": "Seizures in patients with respiratory disease—A retrospective single center study",
"author": "Aydin",
"doi-asserted-by": "crossref",
"first-page": "247",
"journal-title": "Arq. Neuro-Psiquiatr.",
"key": "ref_120",
"volume": "78",
"year": "2020"
},
{
"article-title": "The neurological manifestations of COVID-19: A review article",
"author": "Niazkar",
"first-page": "1667",
"journal-title": "Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol.",
"key": "ref_121",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/j.sapharm.2020.04.001",
"article-title": "Drugs supply and pharmaceutical care management practices at a designated hospital during the COVID-19 epidemic",
"author": "Ying",
"doi-asserted-by": "crossref",
"first-page": "1978",
"journal-title": "Res. Soc. Adm. Pharm. RSAP",
"key": "ref_122",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(20)30203-0",
"article-title": "Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic",
"author": "Rogers",
"doi-asserted-by": "crossref",
"first-page": "611",
"journal-title": "Lancet Psychiatry",
"key": "ref_123",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.1016/j.psym.2020.05.012",
"article-title": "COVID-19 Psychosis: A Potential New Neuropsychiatric Condition Triggered by Novel Coronavirus Infection and the Inflammatory Response?",
"author": "Ferrando",
"doi-asserted-by": "crossref",
"first-page": "551",
"journal-title": "Psychosomatics",
"key": "ref_124",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2020.04.027",
"article-title": "Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms",
"author": "Troyer",
"doi-asserted-by": "crossref",
"first-page": "34",
"journal-title": "Brain Behav. Immun.",
"key": "ref_125",
"volume": "87",
"year": "2020"
},
{
"DOI": "10.1016/j.dscb.2023.100074",
"article-title": "COVID-19 delirium and encephalopathy: Pathophysiology assumed in the first 3 years of the ongoing pandemic",
"author": "Otani",
"doi-asserted-by": "crossref",
"first-page": "100074",
"journal-title": "Brain Disord.",
"key": "ref_126",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1186/s10194-020-01188-1",
"article-title": "Headache characteristics in COVID-19 pandemic-a survey study",
"author": "Uygun",
"doi-asserted-by": "crossref",
"first-page": "121",
"journal-title": "J. Headache Pain",
"key": "ref_127",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.3389/fneur.2023.1149294",
"article-title": "Headache in long COVID as disabling condition: A clinical approach",
"author": "Rodrigues",
"doi-asserted-by": "crossref",
"first-page": "1149294",
"journal-title": "Front. Neurol.",
"key": "ref_128",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1007/s11916-022-01086-y",
"article-title": "Post-COVID Headache: A Literature Review",
"author": "Chhabra",
"doi-asserted-by": "crossref",
"first-page": "835",
"journal-title": "Curr. Pain Headache Rep.",
"key": "ref_129",
"volume": "26",
"year": "2022"
},
{
"DOI": "10.3389/fpsyt.2020.582345",
"article-title": "How Does SARS-CoV-2 Affect the Central Nervous System? A Working Hypothesis",
"author": "Panariello",
"doi-asserted-by": "crossref",
"first-page": "582345",
"journal-title": "Front. Psychiatry",
"key": "ref_130",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1007/s00415-021-10752-x",
"article-title": "Association of CNS demyelination and COVID-19 infection: An updated systematic review",
"author": "Ismail",
"doi-asserted-by": "crossref",
"first-page": "541",
"journal-title": "J. Neurol.",
"key": "ref_131",
"volume": "269",
"year": "2022"
},
{
"DOI": "10.3389/fneur.2022.970383",
"article-title": "COVID-19 and the risk of CNS demyelinating diseases: A systematic review",
"author": "Lotan",
"doi-asserted-by": "crossref",
"first-page": "970383",
"journal-title": "Front. Neurol.",
"key": "ref_132",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.spen.2023.101055",
"article-title": "COVID-19 and the Pandemic-Related Aspects in Pediatric Demyelinating Disorders",
"author": "Gombolay",
"doi-asserted-by": "crossref",
"first-page": "101055",
"journal-title": "Semin. Pediatr. Neurol.",
"key": "ref_133",
"volume": "46",
"year": "2023"
},
{
"article-title": "Para and Post-COVID-19 CNS Acute Demyelinating Disorders in Children: A Case Series on Expanding the Spectrum of Clinical and Radiological Characteristics",
"author": "Khair",
"first-page": "e23405",
"journal-title": "Cureus",
"key": "ref_134",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1080/10790268.2021.1888022",
"article-title": "Spinal cord involvement in COVID-19: A review",
"author": "Garg",
"doi-asserted-by": "crossref",
"first-page": "390",
"journal-title": "J. Spinal Cord Med.",
"key": "ref_135",
"volume": "46",
"year": "2023"
},
{
"DOI": "10.1111/ene.14952",
"article-title": "Systematic review of cases of acute myelitis in individuals with COVID-19",
"author": "Schulte",
"doi-asserted-by": "crossref",
"first-page": "3230",
"journal-title": "Eur. J. Neurol.",
"key": "ref_136",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1016/j.radcr.2020.06.001",
"article-title": "Acute myelitis as a neurological complication of Covid-19: A case report and MRI findings",
"author": "AlKetbi",
"doi-asserted-by": "crossref",
"first-page": "1591",
"journal-title": "Radiol. Case Rep.",
"key": "ref_137",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1007/s00415-020-09934-w",
"article-title": "Acute transverse myelitis after COVID-19 pneumonia",
"author": "Munz",
"doi-asserted-by": "crossref",
"first-page": "2196",
"journal-title": "J. Neurol.",
"key": "ref_138",
"volume": "267",
"year": "2020"
},
{
"DOI": "10.3346/jkms.2020.35.e174",
"article-title": "Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients",
"author": "Lee",
"doi-asserted-by": "crossref",
"first-page": "e174",
"journal-title": "J. Korean Med. Sci.",
"key": "ref_139",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1002/hed.26204",
"article-title": "Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases",
"author": "Vaira",
"doi-asserted-by": "crossref",
"first-page": "1252",
"journal-title": "Head Neck",
"key": "ref_140",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1101/2020.02.22.20026500",
"doi-asserted-by": "crossref",
"key": "ref_141",
"unstructured": "Mao, L.W.M., Chen, S., He, Q., Chang, J., Hong, C., and Hu, B. (2020). Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study. MedRxiv."
},
{
"DOI": "10.1002/alr.22593",
"article-title": "Potential pathogenesis of ageusia and anosmia in COVID-19 patients",
"author": "Vaira",
"doi-asserted-by": "crossref",
"first-page": "1103",
"journal-title": "Int. Forum Allergy Rhinol.",
"key": "ref_142",
"volume": "10",
"year": "2020"
},
{
"article-title": "Neurological manifestations in severe acute respiratory syndrome",
"author": "Tsai",
"first-page": "113",
"journal-title": "Acta Neurol. Taiwanica",
"key": "ref_143",
"volume": "14",
"year": "2005"
},
{
"DOI": "10.1128/JVI.00737-08",
"article-title": "Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2",
"author": "Netland",
"doi-asserted-by": "crossref",
"first-page": "7264",
"journal-title": "J. Virol.",
"key": "ref_144",
"volume": "82",
"year": "2008"
},
{
"DOI": "10.1038/s41368-020-0074-x",
"article-title": "High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Int. J. Oral Sci.",
"key": "ref_145",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/j.1365-2125.2005.02394.x",
"article-title": "Angiotensin II receptor blocker-induces blunted taste sensitivity: Comparison of candesartan and valsartan",
"author": "Tsuruoka",
"doi-asserted-by": "crossref",
"first-page": "204",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "ref_146",
"volume": "60",
"year": "2005"
},
{
"DOI": "10.1007/s00455-013-9487-4",
"article-title": "The effect of barium on perceptions of taste intensity and palatability",
"author": "Dietsch",
"doi-asserted-by": "crossref",
"first-page": "96",
"journal-title": "Dysphagia",
"key": "ref_147",
"volume": "29",
"year": "2014"
},
{
"key": "ref_148",
"unstructured": "Nguyen, T.P., and Taylor, R.S. (2023). Guillain-Barre Syndrome. I, StatPearls Publishing."
},
{
"DOI": "10.1111/jns.12382",
"article-title": "Guillain-Barré syndrome during SARS-CoV-2 pandemic: A case report and review of recent literature",
"author": "Scheidl",
"doi-asserted-by": "crossref",
"first-page": "204",
"journal-title": "J. Peripher. Nerv. Syst. JPNS",
"key": "ref_149",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.17081/innosa.60",
"doi-asserted-by": "crossref",
"key": "ref_150",
"unstructured": "Marenco, A., and Lozada, J.M. (2018). Unusual Clinical Presentation of Guillain Barre Syndrome: A Case Report, Ciencia e Innovación en Salud."
},
{
"DOI": "10.1016/S1474-4422(20)30109-5",
"article-title": "Guillain-Barré syndrome associated with SARS-CoV-2 infection: Causality or coincidence?",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "383",
"journal-title": "Lancet Neurol.",
"key": "ref_151",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1016/j.jneuroim.2020.577294",
"article-title": "Guillain-Barré syndrome in a patient infected with SARS-CoV-2, a case report",
"author": "Farzi",
"doi-asserted-by": "crossref",
"first-page": "577294",
"journal-title": "J. Neuroimmunol.",
"key": "ref_152",
"volume": "346",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2009191",
"article-title": "Guillain-Barré Syndrome Associated with SARS-CoV-2",
"author": "Toscano",
"doi-asserted-by": "crossref",
"first-page": "2574",
"journal-title": "N. Engl. J. Med.",
"key": "ref_153",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1017/cjn.2020.106",
"article-title": "Guillain-Barré Syndrome with Facial Diplegia Related to SARS-CoV-2 Infection",
"author": "Chan",
"doi-asserted-by": "crossref",
"first-page": "852",
"journal-title": "Can. J. Neurol. Sci. J. Can. Sci. Neurol.",
"key": "ref_154",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1016/j.clinph.2020.05.003",
"article-title": "Post SARS-CoV-2 Guillain-Barré syndrome",
"author": "Arnaud",
"doi-asserted-by": "crossref",
"first-page": "1652",
"journal-title": "Clin. Neurophysiol.",
"key": "ref_155",
"volume": "131",
"year": "2020"
},
{
"article-title": "Guillain Barre syndrome associated with COVID-19 infection: A case report",
"author": "Sedaghat",
"first-page": "233",
"journal-title": "J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas.",
"key": "ref_156",
"volume": "76",
"year": "2020"
},
{
"article-title": "Miller Fisher syndrome and polyneuritis cranialis in COVID-19",
"first-page": "e601",
"journal-title": "Neurology",
"key": "ref_157",
"volume": "95",
"year": "2020"
},
{
"article-title": "Does COVID-19 cause axonal GBS?",
"author": "Umapathi",
"first-page": "448",
"journal-title": "J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas.",
"key": "ref_158",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.1016/j.idcr.2020.e00771",
"article-title": "Guillain-Barré syndrome associated with SARS-CoV-2 infection",
"author": "Virani",
"doi-asserted-by": "crossref",
"first-page": "e00771",
"journal-title": "IDCases",
"key": "ref_159",
"volume": "20",
"year": "2020"
},
{
"article-title": "Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): A case report from an Italian COVID-hospital",
"author": "Ottaviani",
"first-page": "1351",
"journal-title": "Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol.",
"key": "ref_160",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/j.neurol.2020.04.007",
"article-title": "Covid-19 and Guillain-Barré syndrome: More than a coincidence!",
"author": "Rafai",
"doi-asserted-by": "crossref",
"first-page": "518",
"journal-title": "Rev. Neurol.",
"key": "ref_161",
"volume": "176",
"year": "2020"
},
{
"DOI": "10.1212/NXI.0000000000000741",
"article-title": "Guillain-Barré syndrome related to COVID-19 infection",
"author": "Alberti",
"doi-asserted-by": "crossref",
"first-page": "e741",
"journal-title": "Neurol. Neuroimmunol. Neuroinflamm.",
"key": "ref_162",
"volume": "7",
"year": "2020"
},
{
"key": "ref_163",
"unstructured": "Organización Mundial de la Salud (2022). Salud Mental y COVID-19: Datos Iniciales Sobre las Repercusiones de la Pandemia, Organización Mundial de la Salud."
},
{
"article-title": "Depression and anxiety during COVID-19 pandemic",
"author": "Nicolini",
"first-page": "542",
"journal-title": "Cir. Cir.",
"key": "ref_164",
"volume": "88",
"year": "2020"
},
{
"DOI": "10.1001/jamapsychiatry.2023.1321",
"article-title": "Neuroinflammation After COVID-19 with Persistent Depressive and Cognitive Symptoms",
"author": "Braga",
"doi-asserted-by": "crossref",
"first-page": "787",
"journal-title": "JAMA Psychiatry",
"key": "ref_165",
"volume": "80",
"year": "2023"
},
{
"key": "ref_166",
"unstructured": "Sadock, B., Sadock, V., and Ruiz, P. (2018). Kaplan y Sadock. Manual de Psiquiatría Clínica, Lippincott Williams & Wilkins (LWW)."
},
{
"article-title": "Actualidades en la fisiopatología del trastorno por estrés postraumático (TEPT)",
"first-page": "128",
"journal-title": "Salud Jalisco",
"key": "ref_167",
"volume": "1",
"year": "2018"
},
{
"key": "ref_168",
"unstructured": "(2024, March 15). Organización Panamericana de la Salud, La Pandemia por COVID-19 Provoca un Aumento del 25% en la Prevalencia de la Ansiedad y la Depresión en todo el Mundo. 6 Marzo 2022. Available online: https://www.paho.org/es/noticias/2-3-2022-pandemia-por-covid-19-provoca-aumento-25-prevalencia-ansiedad-depresion-todo."
},
{
"article-title": "Alteraciones neuropsiquiátricas de la enfermedad por COVID-19",
"first-page": "59",
"journal-title": "Salud Jalisco",
"key": "ref_169",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1176/appi.books.9780890425596",
"doi-asserted-by": "crossref",
"key": "ref_170",
"unstructured": "American Psychiatric Association [APA] (2013). Diagnostic and Statistical Manual of Mental Disorders, Arlington. [5th ed.]."
},
{
"DOI": "10.1136/jnnp-2022-329683",
"article-title": "What is brain fog?",
"author": "McWhirter",
"doi-asserted-by": "crossref",
"first-page": "321",
"journal-title": "J. Neurol. Neurosurg. Psychiatry",
"key": "ref_171",
"volume": "94",
"year": "2023"
},
{
"DOI": "10.1056/NEJMe2400189",
"article-title": "Long Covid and Impaired Cognition—More Evidence and More Work to Do",
"author": "Rosen",
"doi-asserted-by": "crossref",
"first-page": "858",
"journal-title": "N. Engl. J. Med.",
"key": "ref_172",
"volume": "390",
"year": "2024"
},
{
"DOI": "10.1056/NEJMoa2311330",
"article-title": "Cognition and Memory after Covid-19 in a Large Community Sample",
"author": "Hampshire",
"doi-asserted-by": "crossref",
"first-page": "806",
"journal-title": "N. Engl. J. Med.",
"key": "ref_173",
"volume": "390",
"year": "2024"
},
{
"DOI": "10.1016/j.lpm.2021.104090",
"article-title": "Long-COVID: Cognitive deficits (brain fog) and brain lesions in non-hospitalized patients",
"author": "Hugon",
"doi-asserted-by": "crossref",
"first-page": "104090",
"journal-title": "Presse Medicale",
"key": "ref_174",
"volume": "51",
"year": "2022"
},
{
"DOI": "10.1021/acschemneuro.0c00676",
"article-title": "Seeding Brain Protein Aggregation by SARS-CoV-2 as a Possible Long-Term Complication of COVID-19 Infection",
"author": "Tavassoly",
"doi-asserted-by": "crossref",
"first-page": "3704",
"journal-title": "ACS Chem. Neurosci.",
"key": "ref_175",
"volume": "11",
"year": "2020"
}
],
"reference-count": 175,
"references-count": 175,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2227-9059/12/6/1147"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "COVID-19: Unveiling the Neuropsychiatric Maze—From Acute to Long-Term Manifestations",
"type": "journal-article",
"volume": "12"
}